AAOS 2013:超声诊断半月板病变准确性超过MRI
2013-04-04 MedSci MedSci原创
在2013年美国骨科医师学会年会(AAOS)上,来自美国的一项研究报告表明,超声是诊断半月板病变的一个有用工具,其潜在优势超过核磁共振成像(MRI)。 美国密苏里大学James L. Cook博士报告称,MRI通常被认为是半月板异常的金标准诊断显像模式,但它价格昂贵、不易获得大量患者,而且误诊率可达20%。 “超声检查可能是诊断半月板病变的一种有效工具,其潜在性克
在2013年美国骨科医师学会年会(AAOS)上,来自美国的一项研究报告表明,超声是诊断半月板病变的一个有用工具,其潜在优势超过核磁共振成像(MRI)。
美国密苏里大学James L. Cook博士报告称,MRI通常被认为是半月板异常的金标准诊断显像模式,但它价格昂贵、不易获得大量患者,而且误诊率可达20%。
“超声检查可能是诊断半月板病变的一种有效工具,其潜在性克服MRI很多缺点,”他说。“另外,超声仪器携带方便,能够准确诊断可能的运动(损伤)事件。然而,超声临床诊断患者半月板异常的能力还未得到全面评估。”
“如果这一技术能为受伤膝关节半月板病变的特征和诊断始终提供标准化的敏感和特异性数据,那么它将非常有用,” Cook博士接着说,“因为它用于这一领域,所以它常规使用,对患者身高无限制,价格比MRI便宜。”
前瞻性比较
Cook博士和他的同事开展了一项研究,目的是确定在急性膝关节疼痛患者中,超声诊断半月板病变的临床实用性,以及比较超声和MRI临床诊断准确率。经IRB批准的前瞻性研究队列包含了71例急性膝关节疼痛的患者。
术前MRI(1.5T)扫描和超声对每一个受累膝关节都进行检查。MRI由接受过骨骼肌肉MRI培训的放射学医生读片;超声由接受过骨骼肌肉超声检查培训的医生进行读片。骨科医生对每一个受累关节做关节镜评价,用于评估和记录所有关节病变,这可作为半月板病变存在、类型和严重程度的参考标准。
每一种诊断模式的评估者都不知道其他所有资料。而是由一个独立研究者进行资料的收集和比较。结果如表1
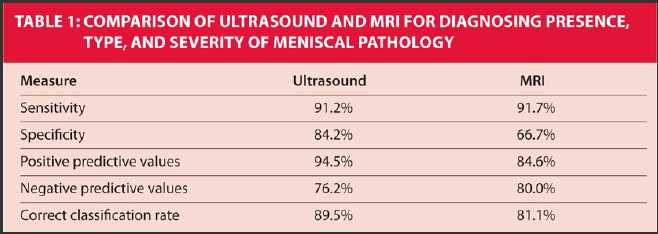
“在这一前瞻性临床研究中,超声在准确确定是否存在半月板病变(关节镜能看到的病变)上可能是MRI的2倍多。”
他总结说,“超声是诊断半月板病变的有用工具,其潜在优势超过MRI。除具有目前仪器的可利用率和携带性外,超声还可作为诊断运动员半月板损伤获得最少伤害的诊断模式。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#AAOS#
0
#准确性#
60
超声很好的优势
156
#AAO#
70
#半月板#
61
#超声诊断#
71
#超声诊断#
65