Nat Commun:孤化学感官细胞是牙周炎的免疫哨兵
2020-04-06 MedSci原创 MedSci原创
孤化学感官细胞(SCCs)是上皮哨兵,它利用苦味Tas2r受体和耦合的味觉转导元件来检测病原菌代谢产物,触发宿主防御,控制感染。在这里,我们报告了SCCs存在于小鼠牙龈结节上皮中,它们表达了几个Tas
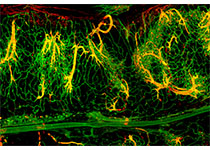
孤化学感官细胞(SCCs)是上皮哨兵,它利用苦味Tas2r受体和耦合的味觉转导元件来检测病原菌代谢产物,触发宿主防御,控制感染。在这里,我们报告了SCCs存在于小鼠牙龈结节上皮中,它们表达了几个Tas2rs和味觉转导成分α-gustducin(Gnat3)、TrpM5和Plcβ2。Gnat3-/-小鼠的口腔共生微生物群发生了改变,并加速了自然发生的牙槽骨损失。
在结扎诱导的牙周炎中,敲除味觉信号分子或基因缺失的牙龈SCCs(gSCCs)会增加细菌负荷,降低细菌多样性,使微生物群更具致病性,导致牙槽骨丧失更大。使用苦味丹激活gSCCs的局部治疗可上调抗菌肽的表达,并改善野生型小鼠结扎诱导的牙周炎,但在Gnat3-/-小鼠中没有。
总之,该研究结果表明,gSCCs可能为治疗牙周炎提供了一个有希望的靶点,通过利用先天免疫调节口腔微生物群来治疗牙周炎。
原始出处:
Xin Zheng, Marco Tizzano, et al., Gingival solitary chemosensory cells are immune sentinels for periodontitis. Nat Commun. 2019; 10: 4496.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
84
#COMMUN#
66
很好的学习机会
121
#牙周#
56
很好的学习机会
130
学习了
115