Circulation/Eur Heart J:欧美多学会相继制定自发性冠脉夹层科学声明:是中青年女性、妊娠期或分娩后心梗常见原因
2018-02-27 岱西 中国循环杂志
近日,Circulation和Euro Heart J分别发布了自发性冠状动脉夹层(SCAD)的科学声明,SCAD是指冠状动脉壁内假腔对真腔产生压迫,进而引起冠脉血流减少导致的病症。
近日,Circulation和Euro Heart J分别发布了自发性冠状动脉夹层(SCAD)的科学声明,SCAD是指冠状动脉壁内假腔对真腔产生压迫,进而引起冠脉血流减少导致的病症。
两份声明结合来看,要点如下:
1.自发性冠状动脉夹层由壁内血肿或内膜断裂导致冠脉阻塞,而非由动脉粥样硬化斑块破裂或腔内血栓所致。
2.自发性冠状动脉夹层有较强的女性倾向性以及与妊娠相关性,提示雌激素在其发病机制或有一定作用。
3.自发性冠状动脉夹层多见于左前降支,发病率在35%~46%;冠脉中远段为常见病变部位;夹层多发于中膜的外1/3。
4.自发性冠状动脉夹层常发生于无传统心血管危险因素的人群中,平均年龄为44~53岁,男性发病年龄或稍小于女性。
5.自发性冠状动脉夹层是中青年女性急性冠脉综合征、妊娠期或分娩后心梗常见原因。
6.自发性冠状动脉夹层是急性心梗及心原性猝死的重要原因。对于不明原因心原性猝死者,事后鉴别诊断应考虑到自发性冠状动脉夹层,并仔细检查整个冠脉。
7.与自发性冠状动脉夹层相关的疾病和因素包括:肌纤维发育不良(最多见);妊娠、多胎分娩(≥4)、遗传性动脉病和结缔组织病(如马凡氏综合征、多囊肾病等)、外源性激素(如口服避孕药、糖皮质激素、绝经后激素代替治疗等)、全身性炎症疾病(如系统性红斑狼疮、克罗恩病、结节性多动脉炎等)、偏头痛、冠脉痉挛等,以及一些诱发因素,如剧烈运动、呕吐、咳嗽、举重物、情绪激动、吸食毒品等。
9.诊断自发性冠状动脉夹层首选冠脉造影。多血管自发性冠状动脉夹层不少见,发病率约为9%~23%,造影时应评估这种可能性。诊断不确定时可考虑光学相干断层成像(OCT)。
注:A:1型,有多个射线可透的腔隙或管壁造影剂充盈的典型征象;B:2型,出现严重程度和长度不同的弥漫性狭窄; C:3型,局灶性或管状狭窄,通常长度<20mm;D:3型OCT成像显示壁内血肿(星号)。
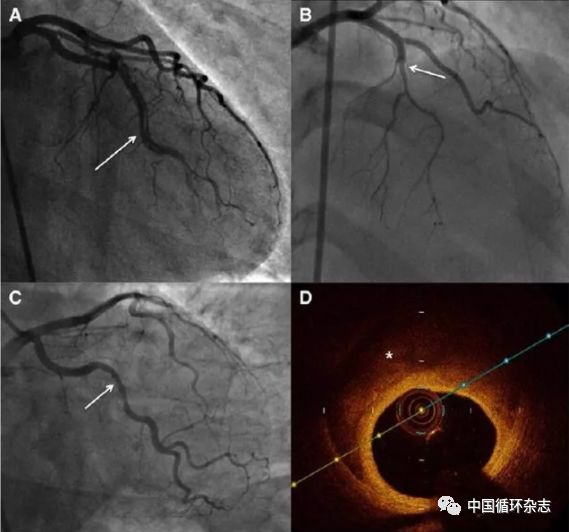
图2 自发性冠状动脉夹层冠脉造影分型
10.与冠心病相比,自发性冠状动脉夹层的冠脉血运重建出现并发症和不良结局的风险更高。自发性冠状动脉夹层的急性和康复期治疗策略可能与动脉粥样硬化性急性心梗有重要差别,还需进一步研究加以明确。
11.药物治疗方面,对于接受双联抗血小板治疗以及阿司匹林治疗仍存争议;对于左心室功能障碍或心律失常以及伴有高血压的自发性冠状动脉夹层患者而言,应考虑使用β阻滞剂;合并左心室功能障碍时,推荐使用ACEI或ARB;不常规推荐使用他汀类药物;对于抗心绞痛药物,使用前需要权衡利弊。
13.由自发性冠状动脉夹层所致心梗患者应接受心脏康复治疗进行二级预防;此外心理疏导,精神护理也是维持近期和远期健康的重要举措。
原始出处:
[1]Hayes SN, Kim ESH, Saw J, et al.Spontaneous Coronary Artery Dissection: Current State of the Science: A Scientific Statement From the American Heart Association.Circulation. 2018 Feb 22. pii: CIR.0000000000000564. doi: 10.1161/CIR.0000000000000564. [Epub ahead of print]
[2]Adlam D, Alfonso F, Maas A,et al.European Society of Cardiology, acute cardiovascular care association, SCAD study group: a position paper on spontaneous coronary artery dissection.Eur Heart J. 2018 Feb 22. doi: 10.1093/eurheartj/ehy080. [Epub ahead of print]
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#自发性冠脉夹层#
86
#妊娠期#
69
#分娩#
71
#ART#
67
#自发性#
0
#HEART#
54
#中青年#
69