PLoS One:A2DS2分数可预测中国缺血性卒中患者卒中相关肺炎和住院死亡
2016-03-14 MedSci MedSci原创
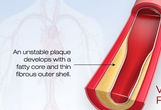
背景和目的:卒中相关性肺炎(SAP)是常见的并发症,并且也是住院期间死亡的重要原因之一。A2DS2(年龄、心房纤颤、吞咽困难、性别、卒中的严重程度)评分是柏林卒中注册开发,能够很好的预测SAP的发生。研究者旨在识别A2DS2评分和SAP之间的关联,并且确定A2DS2评分是否能预测中国人群急性缺血性卒中的死亡。方法:研究者进行了一项回顾性的研究。将1239名急性缺血性脑卒中患者分为低A2DS2组(0
背景和目的:卒中相关性肺炎(SAP)是常见的并发症,并且也是住院期间死亡的重要原因之一。A2DS2(年龄、心房纤颤、吞咽困难、性别、卒中的严重程度)评分是柏林卒中注册开发,能够很好的预测SAP的发生。研究者旨在识别A2DS2评分和SAP之间的关联,并且确定A2DS2评分是否能预测中国人群急性缺血性卒中的死亡。
方法:研究者进行了一项回顾性的研究。将1239名急性缺血性脑卒中患者分为低A2DS2组(0-4)和高A2DS2评分(5-10)组。主要预后为住院卒中相关肺炎的发生,应用Logistic回归分析确定A2DS2评分和SAP之间的关联,以及A2DS2评分和住院死亡的相关性。
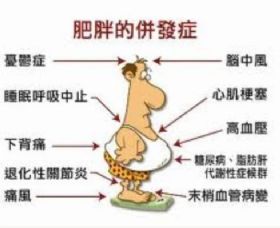
结果:急性缺血性卒中后,SAP和住院死亡率的总体发生率分别为7.3%和2.4%的。低SAP组和高A2DS2评分组卒中相关性肺炎的发生率分别为3.3%和24.7%(P<0.001)。在住院期间,1.2%低评分组的患者和7.8%高分组的患者死亡。多元回归分析显示,高评分组患者卒中相关肺炎(OR 8.888, 95%CI:5.552-14.229)和死亡(OR 7.833,95% CI:3.580-17.137)的发生风险高于低评分组的患者。
结论:A2DS2评分是中国急性缺血性患者,卒中相关性肺炎和住院死亡的强预测因子。A2DS2评分可能是预测住院期间发生SAP和死亡的有效评分。
原文出处:
Zhang X1, Yu S2,et al. The A2DS2 Score as a Predictor of Pneumonia and In-Hospital Death after Acute Ischemic Stroke in Chinese Populations. PLoS One. 2016 Mar 7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#A2DS2分数#
61
#缺血性卒#
67
#A2DS2分数#
55
#缺血性#
56
#Plos one#
63
#卒中患者#
59
#缺血性卒中患者#
50