Blood:如何治疗伯基特淋巴瘤
2018-07-07 月下荷花 肿瘤资讯
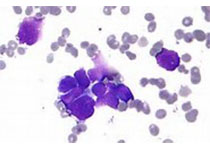
在非洲,伯基特淋巴瘤(BL)是最常见的儿童癌症,也常发生于青少年和青年人(AYA),多与人免疫缺陷病毒(HIV)有关。来自马拉维的Gopal教授在BLOOD杂志上对非洲BL诊断、前期治疗及根治性治疗进行了总结。非洲属于非高收入地区,很多治疗与想法虽然有其局部特色,但值得借鉴与思考。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习
109
学习
118
#伯基特淋巴瘤#
71
学习
101
学习
124
学习了.谢谢分享
129
学习了.谢谢分享
48
学习了.有用
64
学习了很有用不错
75
了解一下.谢谢分享!
55