超声引导桡动脉穿刺,你需要掌握这些技巧!
2017-01-07 丛海涛 医学界麻醉频道
盲法穿刺有时需多次尝试才能成功,这易使患者不适,并导致出血及动脉痉挛等。对医生来说,盲法插管也是一个很大的挑战,超声引导下可视穿刺置管效果更好。如何正确应用横断面定位(短轴)及纵向定位下(长轴)超声引导的可视桡动脉插管?本文将为您详细介绍:正常桡动脉的超声图像:超声下正常桡动脉纵轴呈长管状,边界整齐, 自近心端向远心端内径逐渐变细。我们常常称之为“双轨征”。 &
盲法穿刺有时需多次尝试才能成功,这易使患者不适,并导致出血及动脉痉挛等。对医生来说,盲法插管也是一个很大的挑战,超声引导下可视穿刺置管效果更好。如何正确应用横断面定位(短轴)及纵向定位下(长轴)超声引导的可视桡动脉插管?本文将为您详细介绍:
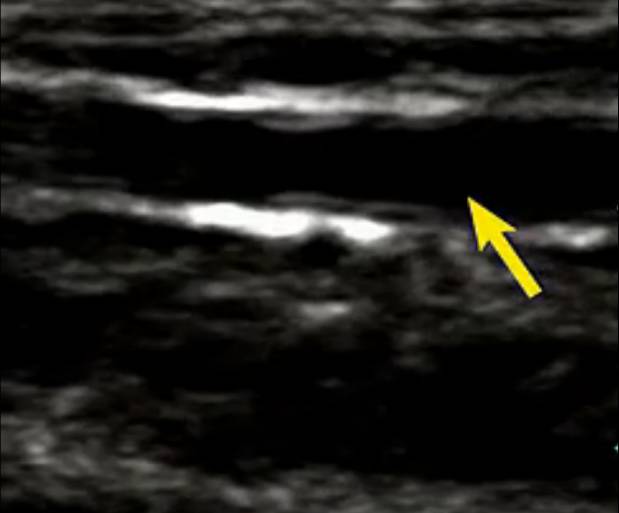
正常桡动脉的超声图像:超声下正常桡动脉纵轴呈长管状,边界整齐, 自近心端向远心端内径逐渐变细。我们常常称之为“双轨征”。


关于桡动脉的直径,有研究结果发现成人患者右侧桡动脉远端直径的范围为1.3 mm~3.6 mm(桡动脉直径的测量点位于桡骨茎突近端1cm)处,平均直径为2.38±0.56 mm。其中,男性右侧桡动脉直径明显大于女性 (2.47±0.57 mm VS 2.17±0.48 m, P < 0.01) 。左侧桡动脉与右侧桡动脉直径无统计学差异。
正常桡动脉频谱为动脉频谱,表现为收缩早期血流速度加快,形成陡直的向上波峰,然后迅速下降。正常桡动脉的内膜光滑,较薄,平均内膜厚度为0.25±0.12 mm。
留置针置入后,可能会出现扭曲、打折,因此尽量先选择近腕部、远肘部的位置穿刺。患者移动或更换体位时都可能引起导管的上述异常。
确定桡动脉后,进一步调整,使血管与周围组织对比更分明。调整深度,使桡动脉成像处于屏幕中央位置,清晰可见。从腕部扫描至肘窝,注意观察是否存在动脉迂曲及钙化。穿刺部位则选在血管直径最大及钙化程度最低部位。不需要像盲法穿刺时选择的固定位置,这也是可视化穿刺的一大优势,可以选择任何一个适合的穿刺点。
根据超声显示桡动脉不同平面,超声定位下桡动脉穿刺分为平面外法和平面内法。
平面外法:确定穿刺点后,移动探头位置使桡动脉成像处于屏幕中央位置。对穿刺部位皮肤进行局部麻醉后,以45°~60°角插入留置针。轻微抖动留置针,并调整探头保证针头在屏幕上清晰显影。

针尖向动脉推进过程中,注意倾斜探头,保证针尖一直可见。每隔一定时间确定针尖位置,保证其一直在动脉血管上方,穿刺针进入血管腔后,检查有无血液回流,确定针尖位置正确。

调整留置针至水平,以再次确定针尖位于血管内。保持穿刺针针尖位置不变,将套管继续向前推进,其后撤出穿刺针针芯,并将压力传感器与留置针套管连接。

平面内法:超声波探头纵向确定血管位置。桡动脉成像处于屏幕中央位置后,旋转探头90°。在屏幕中央可见动脉,可见长轴及血管最大直径处。

以15°~30°角进针,使针尖与血管长轴保持平行向前推进。如果屏幕上不见针头显影,其可能是在血管壁或血管外,回撤穿刺针,但不完全撤出,只调整角度使针尖显影可见于屏幕。再次向前推进,直至其进入管腔,并见回血。保持穿刺针针芯位置不变,将外套管继续向前推进,其后撤出穿刺针针芯,并将压力传感器与留置针套管连接。

超声引导下桡动脉可视穿刺置管的主要挑战在于鉴别针尖和针体,其在屏幕上都以白点显示。缺少经验的医师认为的显影通常来自针体,而针尖很可能已经穿过动脉,引起深部组织损伤。
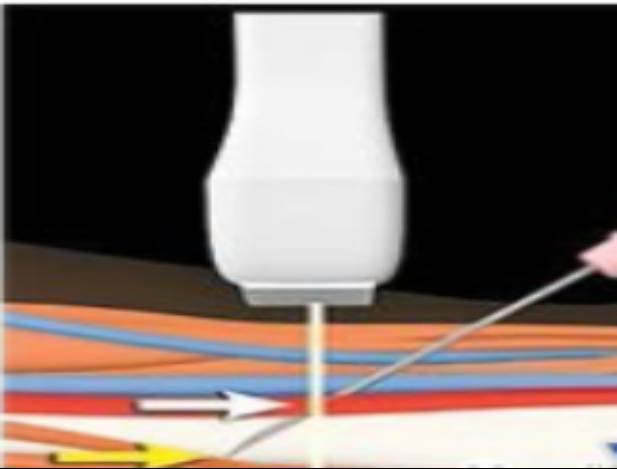
因此,在插入穿刺针时,要保证针尖一直可见。可以采用抖动穿刺针的方法和移动探头找针的方法确定针尖的位置。
问题来了——
1
同一部位反复穿刺不成功的原因有哪些?
(1)未能击中桡动脉:首先分析穿刺失败的可能原因,针对不同情况改变穿刺手法后进针,例如对于较硬易于滑动的桡动脉,患者的动脉搏动很强,但难以击中,穿刺时适当加大进针的角度和速度常有助于刺中桡动脉;相反对于桡动脉较细、搏动较弱的患者,应小角度穿刺,同时缓慢进针常有利于穿刺成功。
(2)穿刺部位桡动脉走行迂曲:通常在这种情况下难以保证穿刺时的进针方向与桡动脉走行一致,因此穿刺难以成功,多需要更换穿刺点至桡动脉走行较直部位后再行穿刺。
(3)桡动脉发生痉挛:这种情况下常表现为桡动脉的搏动减弱甚至消失,此时选择盲目穿刺可能会进一步加重桡动脉痉挛的程度,等待桡动脉搏动恢复后再行穿刺或许是更为明智的选择,也有学者认为皮下给予硝酸甘油有助于缩短桡动脉痉挛后的恢复时间。
(4)穿刺局部形成血肿:此种情况下在原部位继续穿刺很难获得成功,应避开血肿部位后重新选择穿刺点。
2
穿刺针刺入桡动脉但针尾部血流不畅原因是?
(1)穿刺针尖斜面未完全进入血管腔:在这种情况下,针尖的位置可能位于桡动脉的前壁或后壁,操作者常可通过调整穿刺针的深度和进针角度使针尖完全进入血管腔。
(2)桡动脉痉挛:动脉痉挛后导致搏动减弱,同时血流量减少,血压降低,触摸搏动困难同时即使击中后血流也不顺畅。
(3)穿刺针进入桡动脉分支:在调整穿刺针位置后仍无法顺利置管,穿刺点过于靠近腕部时多见,常需要向近心端前移穿刺点后再次进针。
3
动脉痉挛如何处理?
桡动脉穿刺置管中会遇见的一挑战是动脉痉挛,使进针存在阻力同时击中动脉后针尾部血流不畅。如果发生动脉痉挛,最好在近心端重新确定穿刺点或应换至对侧手臂。
4
应用超声平面内和平面外法有何优缺点?
平面内优点是全程可以看到穿刺针的运动轨迹,容易确立穿刺的深度。缺点是由于超声是二维图像,容易产生切片厚度伪像问题,看到穿刺针在血管内却见不到血液回流,说明针可能紧邻血管壁,同时也容易导致置管失败。
平面外的优点是可以从动脉的正上方穿刺,容易确定穿刺的方向缺点是不容易鉴别针尖和针体,需要不断移动探头,找到穿刺针针尖是操作的关键。可以联合平面内观察针尖的位置。
5
穿刺置管失败你将如何处理?
①压迫止血,等待搏动恢复再穿刺或者更换穿刺点;
②对于无搏动的情况有经验的操作者可以选用解剖穿刺法;
③选择对侧桡动脉,或者选择肱动脉、足背动脉、 股动脉等;
④换成小一号的穿刺针降低穿刺难度;
⑤应用有导丝的动脉专用穿刺针;
⑥应用超声定位下穿刺;
⑦求助上级医师。
⑧求助外科医师切开置管。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#桡动脉穿刺#
74
#超声引#
56
#超声引导#
50
#穿刺#
54
#桡动脉#
67