重磅!Nat Med报道HIV抗体临床实验获得成功
2017-01-20 佚名 生物谷
一个由洛克菲勒大学研究人员和科隆大学及德国感染研究中心的Florian Klein教授领导的研究团队在人体中检测了一个新的HIV中和抗体(10-1074)的效果,相关临床试验数据最近发表在《Nature Medicine》上。 过去几年里,研究人员发现了一些新的HIV中和抗体。“这些抗体作用很强大,可有效中和一系列不同的HIV病毒株,因此它们在发展HIV疫苗过程中发挥重要作用。”Klei
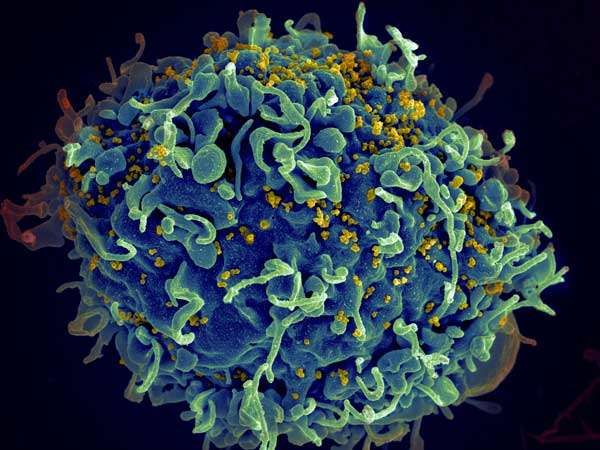
一个由洛克菲勒大学研究人员和科隆大学及德国感染研究中心的Florian Klein教授领导的研究团队在人体中检测了一个新的HIV中和抗体(10-1074)的效果,相关临床试验数据最近发表在《Nature Medicine》上。
过去几年里,研究人员发现了一些新的HIV中和抗体。“这些抗体作用很强大,可有效中和一系列不同的HIV病毒株,因此它们在发展HIV疫苗过程中发挥重要作用。”Klein教授说道。此外,通过与科隆大学医院传染病科及洛克菲勒大学的研究人员合作,Klein教授正在研究这些广谱中和性抗体是否可以用于治疗HIV感染。
广谱中和抗体10-1074可靶向HIV衣壳蛋白上的一个特殊结构。在这项研究中,研究人员发现病人对该抗体具有很好的耐受性,其药代动力学性质也很好。此外,研究人员发现该抗体在HIV感染者身上表现出了很高的抗病毒活性。研究团队还以此研究了耐药性HIV变异株的发展过程。“我们对HIV序列进行了全面分析,以确定HIV逃过抗体产生的选择压力的过程及机理。”该论文的共同第一作者之一Henning Gruell博士说道。
“这项研究在洛克菲勒大学和许多其他研究机构合作者的紧密合作下取得了成功。”Klein教授说道,他是德国的项目负责人,也是这篇论文的共同通讯作者之一。该研究团队正在计划进一步的临床实验以研究该抗体介导的免疫反应对HIV感染者的治疗效果,计划在春季进行接下来的临床实验。
原始出处:Antibody 10-1074 suppresses viremia in HIV-1-infected individuals,Marina Caskey et al, Nature Medicine (2017).DOI: 10.1038/nm.4268。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#HIV抗体#
71
#Nat#
59
#临床实验#
63
长见识了,厉害
95
#重磅#
58
#Med#
71
长长见识了!
101