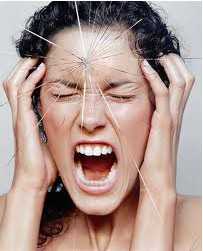
The EMBO J:研究者揭示慢性疼痛中天然蛋白质14-3-3ζ的重要作用
2012-06-17 T.Shen 生物谷
近日,来自法国和瑞典的研究者发现大鼠机体的蛋白质是如何介导产生慢性疼痛感的。相关研究成果刊登在了国际著名杂志EMBO Journal上。慢性疼痛具有持续性,而且经常很难处理,部分是因为神经元分子信号发生的改变,这种改变最终会破坏神经信号从脊椎到大脑的传递。研究者Marc表示,他们运用一系列的技术更精确地从分子水平来研究导致动物慢性疼痛的分子机制。 研究结果揭示了天然蛋白质14-3-3ζ在慢性疼痛

近日,来自法国和瑞典的研究者发现大鼠机体的蛋白质是如何介导产生慢性疼痛感的。相关研究成果刊登在了国际著名杂志EMBO Journal上。慢性疼痛具有持续性,而且经常很难处理,部分是因为神经元分子信号发生的改变,这种改变最终会破坏神经信号从脊椎到大脑的传递。研究者Marc表示,他们运用一系列的技术更精确地从分子水平来研究导致动物慢性疼痛的分子机制。
研究结果揭示了天然蛋白质14-3-3ζ在慢性疼痛的大鼠脊椎中水平较高,而且研究者揭示了14-3-3ζ蛋白质可以引发信号途径的改变进而引发慢性疼痛症状出现。14-3-3ζ蛋白质可以破坏GABA-B受体两个亚基之间的相互作用,GABA-B受体是在神经细胞表面发现的蛋白质复合物。GABA-B受体是G蛋白偶联受体。研究者使用抗体标记和显微镜技术来研究信号蛋白之间的分子反应,在细胞和活的动物体内,研究者揭示了14-3-3ζ蛋白质可以直接和GABA-B受体的B1亚基反应,这种反应损害了受体的信号效用,而且限制了疼痛感的释放。
研究者同时也揭示了用一种特殊的小感染RNA(siRNA)技术或者竞争肽来治疗大鼠的疗法。通过14-3-3ζ蛋白质引发的GABA-B受体损伤对于调节慢性疼痛是一种新的机制。研究者表示,我们可以用抑制剂来干扰蛋白质14-3-3ζ的功能,从而提出新的疗法。以GABA-B受体分散过程为靶标也可以成为治疗的靶点,这将使得标准的止痛药发挥更大的药效。(生物谷Bioon.com)
编译自:Naturally Occurring Protein Has Role in Chronic Pain
编译者:T.Shen

doi:10.1038/emboj.2012.161
PMC:
PMID:
Impairment of GABAB receptor dimer by endogenous 14-3-3ζ in chronic pain conditions
Sophie Laffray, Rabia Bouali-Benazzouz, Marie-Amélie Papon, Alexandre Favereaux, Yang Jiang, Tina Holm, Corentin Spriet, Pascal Desbarats, Pascal Fossat, Yves Le Feuvre, Marion Decossas, Laurent Héliot, Ulo Langel, Frédéric Nagy and Marc Landry
In the central nervous system, the inhibitory GABAB receptor is the archetype of heterodimeric G protein-coupled receptors (GPCRs). However, the regulation of GABAB dimerization, and more generally of GPCR oligomerization, remains largely unknown. We propose a novel mechanism for inhibition of GPCR activity through de-dimerization in pathological conditions. We show here that 14-3-3ζ, a GABAB1-binding protein, dissociates the GABAB heterodimer, resulting in the impairment of GABAB signalling in spinal neurons. In the dorsal spinal cord of neuropathic rats, 14-3-3ζ is overexpressed and weakens GABAB inhibition. Using anti-14-3-3ζ siRNA or competing peptides disrupts 14-3-3ζ/GABAB1 interaction and restores functional GABAB heterodimers in the dorsal horn. Importantly, both strategies greatly enhance the anti-nociceptive effect of intrathecal Baclofen in neuropathic rats. Taken together, our data provide the first example of endogenous regulation of a GPCR oligomeric state and demonstrate its functional impact on the pathophysiological process of neuropathic pain sensitization.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#研究者#
67
#白质#
76
#重要作用#
68
#慢性疼痛#
70
#蛋白质#
67