Sci. Transl. Med.:磷脂带来多发性硬化症治疗新希望
2012-06-17 bo 生物谷
6月6日,Sci. Transl. Med.杂志报道了磷脂可成为多发性硬化症(MS)治疗的新希望。脂类构成髓鞘的70%组分,而针对脂类的自身抗体可造成多发性硬化症的特征性变化:脱髓鞘反应。 研究者应用脂类抗原微阵列和脂类质谱技术,在MS患者大脑内发现了自身免疫反应真正的脂类靶向物。他们还用一种MS动物模型研究了这些脂类靶向物在自身免疫脱髓鞘过程中的作用。 研究发现,MS患者体内的自身抗体,靶向
6月6日,Sci. Transl. Med.杂志报道了磷脂可成为多发性硬化症(MS)治疗的新希望。脂类构成髓鞘的70%组分,而针对脂类的自身抗体可造成多发性硬化症的特征性变化:脱髓鞘反应。
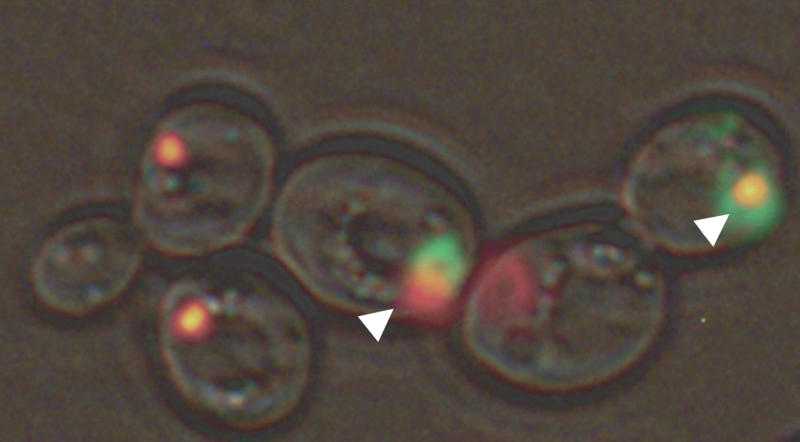
研究者应用脂类抗原微阵列和脂类质谱技术,在MS患者大脑内发现了自身免疫反应真正的脂类靶向物。他们还用一种MS动物模型研究了这些脂类靶向物在自身免疫脱髓鞘过程中的作用。
研究发现,MS患者体内的自身抗体,靶向磷脂酰丝氨酸和氧化卵磷脂衍生物中的一个磷酸基团。给予这些脂类的治疗,可通过抑制自身免疫反应和诱导自身反应T细胞缓解实验性自身免疫性脑脊髓炎。这样的效果是由脂类饱和脂肪酸侧链介导的。因此,磷脂看作为天然抗炎复合物,具有治疗MS的良好前景。(生物谷bioon.com)

doi:10.1016/j.cell.2011.10.017
PMC:
PMID:
Identification of Naturally Occurring Fatty Acids of the Myelin Sheath That Resolve Neuroinflammation
Peggy P. Ho1,*, Jennifer L. Kanter1,2,*, Amanda M. Johnson1,2, Hrishikesh K. Srinagesh1, Eun-Ju Chang2,3, Timothy M. Purdy2,3, Keith van Haren1,2,3, William R. Wikoff4, Tobias Kind4, Mohsen Khademi5, Laura Y. Matloff1, Sirisha Narayana1,2, Eun Mi Hur1, Tamsin M. Lindstrom2,3, Zhigang He6, Oliver Fiehn4, Tomas Olsson5, Xianlin Han7, May H. Han1, Lawrence Steinman1,*,? and William H. Robinson2,3,*,?
Lipids constitute 70% of the myelin sheath, and autoantibodies against lipids may contribute to the demyelination that characterizes multiple sclerosis (MS). We used lipid antigen microarrays and lipid mass spectrometry to identify bona fide lipid targets of the autoimmune response in MS brain, and an animal model of MS to explore the role of the identified lipids in autoimmune demyelination. We found that autoantibodies in MS target a phosphate group in phosphatidylserine and oxidized phosphatidylcholine derivatives. Administration of these lipids ameliorated experimental autoimmune encephalomyelitis by suppressing activation and inducing apoptosis of autoreactive T cells, effects mediated by the lipids’ saturated fatty acid side chains. Thus, phospholipids represent a natural anti-inflammatory class of compounds that have potential as therapeutics for MS.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#多发性#
46
#Transl#
66
#TRA#
70
#新希望#
70
#Transl.#
48
#硬化症#
76
#Med#
56