Ann Surg:溃疡性结肠炎结肠切除术后回肠直肠吻合术的长期随访结果
2016-10-15 MedSci MedSci原创
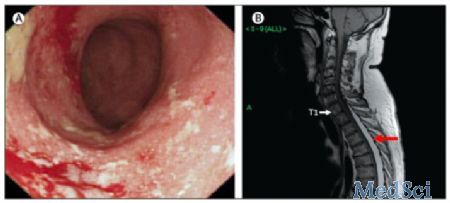
确定溃疡性结肠炎(UC)结肠切除术后回肠直肠吻合术(IRA)失败的累计发病率和预后因素。虽然推荐UC患者结肠切除术后行回肠袋-肛管吻合术,但仍在进行IRA操作。这是一项多中心回顾性队列研究,包括在1960和2014年之间,进行IRA的UC患者。IRA失败定义为二次直肠切除术和或发生直肠癌。采用Cox比例风险模型进行单、多因素分析。总共有343名患者,来自13个法国中心。IRA后中位随访10.6年。
确定溃疡性结肠炎(UC)结肠切除术后回肠直肠吻合术(IRA)失败的累计发病率和预后因素。
虽然推荐UC患者结肠切除术后行回肠袋-肛管吻合术,但仍在进行IRA操作。
这是一项多中心回顾性队列研究,包括在1960和2014年之间,进行IRA的UC患者。IRA失败定义为二次直肠切除术和或发生直肠癌。采用Cox比例风险模型进行单、多因素分析。
总共有343名患者,来自13个法国中心。IRA后中位随访10.6年。术后10年和20年的IRA失败率为27.0% (95% CI, 22-32) and 40.0% (95% CI 33-47)。非IRA失败者的中位生存时间是26.8年。三分之二的二次直肠切除术是因为难治性直肠炎,20%是因为直肠腺瘤。
单因素分析确定了与IRA失败有关的因素:2005年后进行IRA,IRA时疾病持续时间更长,IRA前使用免疫调节剂治疗。在多变量分析中,结肠切除术前免疫抑制治疗(IS)和抗肿瘤坏死因子治疗,与IRA失败独立相关(HR=2.9, 95% CI 1.2-7.1)。相反,重症急性结肠炎行结肠切除术,可以减少IRA失败率(HR=0.6, 95% CI 0.4-0.97)。
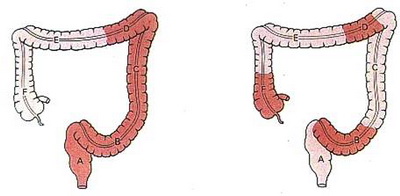
UC患者的IRA失败率很高,尤其是难治性疾病行结肠切除术。不过,对于重症急性结肠炎或之前没有进行IS和抗TNF治疗的患者,可以考虑结肠切除术后行IRA。
原始出处:
Uzzan, Mathieu MD; Cosnes, Jacques MD; Amiot, Aurélien MD; Gornet, Jean-Marc MD; Seksik, Philippe MD; Cotte, Eddy MD; Tiret, Emmanuel MD; Panis, Yves MD; Treton, Xavier MD.Long-term Follow-up After Ileorectal Anastomosis for Ulcerative Colitis: A GETAID/GETAID Chirurgie Multicenter Retrospective Cohort of 343 Patients.Annals of Surgery:
Post Author Corrections: September 21, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#随访结果#
43
#切除术#
50
#吻合术#
0
#结肠切除术#
71
#长期随访#
55
#溃疡性#
52
#回肠#
50