J Thromb Haemost:院前抗血小板治疗与COVID-19住院患者生存率之间的关联
2021-09-12 MedSci原创 MedSci原创
这项迄今为止对COVID-19患者进行院前抗血小板治疗的最大规模观察性研究结果表明其与院内死亡率显著降低有关。
2019冠状病毒病(COVID-19)与高凝状态和血栓形成风险增加有关。院前抗血小板治疗对院内死亡率的影响尚未明确。
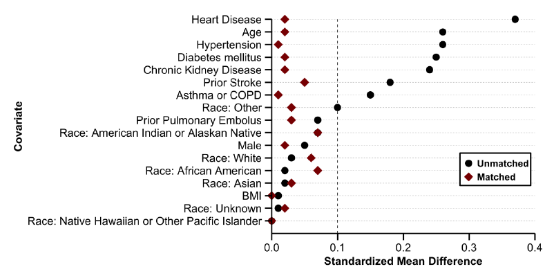
 近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,这项对来自美国90个卫生系统的34675名50岁以上患者进行了观察性队列研究。患者在2020年2月至2020年9月期间经实验室检查确诊COVID-19而住院。对于所有患者,研究人员使用人口统计学和合并症计算接受院前抗血小板治疗的倾向,并根据倾向评分匹配患者,以比较抗血小板组和非抗血小板组的住院死亡率。
近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,这项对来自美国90个卫生系统的34675名50岁以上患者进行了观察性队列研究。患者在2020年2月至2020年9月期间经实验室检查确诊COVID-19而住院。对于所有患者,研究人员使用人口统计学和合并症计算接受院前抗血小板治疗的倾向,并根据倾向评分匹配患者,以比较抗血小板组和非抗血小板组的住院死亡率。
倾向评分匹配的17347名患者队列分别由抗血小板和非抗血小板治疗组的6781名和10566名患者组成。接受院前抗血小板治疗的患者院内死亡率显著降低(18.9% vs. 21.5%,p<0.001),导致死亡率绝对降低2.6%(HR为0.81,95%CI为0.76-0.87,p<0.005)。
一般而言,需要治疗39名患者以防止1例院内死亡。在抗血小板治疗组中,肺栓塞发生率显著降低(2.2% vs. 3.0%,p=0.002),而鼻衄发生率较高(0.9% vs. 0.4%,p<0.001)。其他出血性或血栓性并发症的发生率没有差异。
由此可见,这项迄今为止对COVID-19患者进行院前抗血小板治疗的最大规模观察性研究结果表明其与院内死亡率显著降低有关。需要在基线合并症发生率高的不同患者人群中进行随机对照试验,以确定抗血小板治疗在COVID-19中的最终效果。
原始出处:
Jonathan H. Chow.et al.Association of Pre-Hospital Antiplatelet Therapy with Survival in Patients Hospitalized with COVID-19: A Propensity Score-Matched Analysis.Journal of Thrombosis and Haemostasis.2021.https://onlinelibrary.wiley.com/doi/10.1111/jth.15517
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#院前#
80
#患者生存#
72
#HAE#
60
#生存率#
66
#梅斯医学科研互助群#学习
95
学习了
79
写的不错
94