J Hypertens:踝肱指数可预测靶器官损害
2016-06-18 MedSci MedSci原创
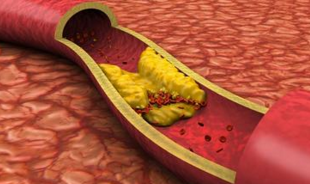
背景:动脉硬化与脑微出血(CMBS)的发病有关。踝肱指数(ABI)可用来预测动脉硬化。研究者假设,由于动脉僵硬度增加和波反射,ABI随年龄的增加而升高,,因而损伤靶器官。本研究旨在探讨ABI与臂踝脉搏波传导速度(baPWV),和CMBS的关系。方法:研究者招募了990名无心血管病和无卒中的受试者[平均年龄53(24-86)岁,531为女性],对所有受试者行颅脑MRI、ABI、baPWV检查。结果:
背景:动脉硬化与脑微出血(CMBS)的发病有关。踝肱指数(ABI)可用来预测动脉硬化。研究者假设,由于动脉僵硬度增加和波反射,ABI随年龄的增加而升高,,因而损伤靶器官。本研究旨在探讨ABI与臂踝脉搏波传导速度(baPWV),和CMBS的关系。
方法:研究者招募了990名无心血管病和无卒中的受试者[平均年龄53(24-86)岁,531为女性],对所有受试者行颅脑MRI、ABI、baPWV检查。
结果:CMBS的患病率为4%。患CMBS的患者ABI(1.14 vs. 1.10)和baPWV(17.29 vs. 14.68 m/s)明显高于没有CMBS。存在CMB的baPWV和ABI的界值分别为1.12和16.07 米/秒。多因素Logistic回归分析显示,ABI高于1.12 [OR:2.57,95% CI 1.30-5.37 ]和baPWV高于16.07 米/秒(OR 2.08,95% CI 1.02-4.38)与CMBS独立相关。此外, ABI高于1.12和baPWV高于 16.07 米/秒的组合与CMBS密切相关(OR 5.26,95% CI 1.93-16.92,P < 0.05)。
结论:高于正常的ABI联合高baPWV与CMBS密切相关,表明ABI可用于预测靶器官损害。
原始出处:
Kinjo Y, Ishida A, et al. A high normal ankle-brachial index combined with a high pulse wave velocity is associated with cerebral microbleeds. J Hypertens. 2016 May 31.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PE#
70
#TENS#
88
#靶器官#
66
#器官损害#
82
好文,值得推荐。
90