Cell:eRNA在调节基因表达中发挥着至关重要作用
2017-01-15 佚名 生物谷
在细胞中,DNA经转录产生RNA,而RNA为细胞表达蛋白提供遗传指令。基因组的大部分经转录产生RNA,但是仅有一小部分RNA确实是来自基因组的蛋白编码区域。 美国宾夕法尼亚大学佩雷尔曼医学院宾州表观遗传学研究所主任、细胞与发育生物学教授Shelley Berger博士说,“为什么非编码区域会发生转录?它们的功能是未知的。” Berger、她的实验室博士后研究员Daniel Bose博士
美国宾夕法尼亚大学佩雷尔曼医学院宾州表观遗传学研究所主任、细胞与发育生物学教授Shelley Berger博士说,“为什么非编码区域会发生转录?它们的功能是未知的。”
Berger、她的实验室博士后研究员Daniel Bose博士研究了增强子对基因表达的调节。增强子是基因组的非编码区域,与基因组的蛋白编码区域相隔较远。增强子提高附近的蛋白编码基因的表达率,因此细胞产生更多的所需的蛋白分子。非编码RNA的一小部分是神秘的增强子RNA(enhancer RNA, eRNA)。它们是由增强子序列经转录而产生的。尽管它们在促进基因表达时起着重要的作用,但是它们如何实现这一点是完全未知的。
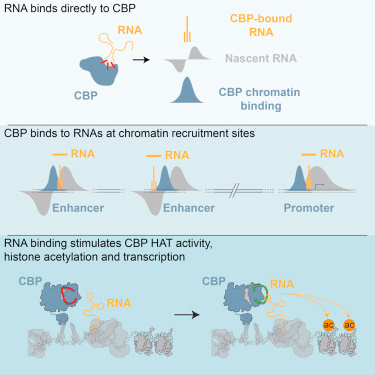
为了获得关于这些神秘的eRNA的新认识,研究人员证实作为一种激活增强子转录的酶,CBP直接结合到eRNA上。这种简单的行为通过调节乙酰化而控制着有机体中的基因表达模式。乙酰化是一种指导在细胞核中紧密包裹的DNA松弛下来促进转录的化学标记。相关研究结果发表在2017年1月12日那期Cell期刊上,论文标题为“RNA Binding to CBP Stimulates Histone Acetylation and Transcription”。
Bose说,“我们体内的细胞具有相同的基因和DNA序列,仅在这些基因如何表达上存在差异。增强子和eRNA在这个过程中发挥着至关重要的作用。我们的研究发现了eRNA产生这些不同的基因表达模式的一个令人兴奋的新方式。我们想知道eRNA是否直接与CBP结合,结果发现它们确实如此。”
利用生化检测方法,他们证实CBP结合到eRNA上的区域也能够调节着CBP加入乙酰化化学标记的能力。通过结合到CBP的这个区域,eRNA能够直接地激活CBP的乙酰化活性。
Berger说,“在癌症生物学世界,人们对增强子和eRNA越来越关注,这是因为存在缺陷的增强子能够导致太多的或太少的蛋白表达,或者能够导致蛋白编码区关闭或启动,或者能够导致蛋白在错误的时间表达。”鉴于近期对人肿瘤进行的DNA测序结果表明与癌症和其他疾病相关的多种突变发生于基因组的增强子区域而不是蛋白编码区域,因此更多地了解增强子和eRNA如何发挥功能将有助于肿瘤学家。
Berger说,“事实上,这是比较重要的,这是因为我们证实eRNA在整个基因组中和体内指导蛋白表达中发挥着关键性作用。我们在全基因组中鉴定出eRNA是结合到CBP上的最为常见的RNA类型,而且鉴定出通过这种相互作用,eRNA在调节CBP活性和基因表达中发挥着一种至关重要的作用。”
Daniel A. Bose, Greg Donahue, Danny Reinberg, Ramin Shiekhattar, Roberto Bonasio, Shelley L. Berger.RNA Binding to CBP Stimulates Histone Acetylation and Transcription.Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#重要作用#
68
#CEL#
76
#eRNA#
64
#Cell#
72
#基因表达#
74