Respirology:前额传感器测量血氧更接近于动脉血水平
2013-06-18 Respirology dxy
A图为指套组传感器和动脉化毛细血管组的氧饱和度Bland-Altman一致性分析图。B图为前额传感器组和动脉化毛细血管组的氧饱和度Bland-Altman一致性分析图。空心圆代表静息状态下收集的数据,实心圆代表运动试验末期收集的数据。图中实线代表差值均数(-2%),虚线代表95%一致性界限(± 3%)。 COPD的血氧测定一般是通过脉搏血氧饱和度仪的指套传感器来测定,但是指套传感器在测量外
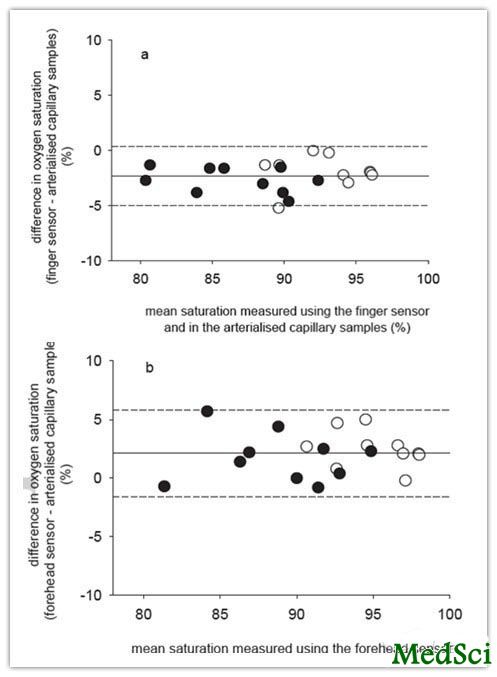
A图为指套组传感器和动脉化毛细血管组的氧饱和度Bland-Altman一致性分析图。B图为前额传感器组和动脉化毛细血管组的氧饱和度Bland-Altman一致性分析图。空心圆代表静息状态下收集的数据,实心圆代表运动试验末期收集的数据。图中实线代表差值均数(-2%),虚线代表95%一致性界限(± 3%)。
COPD的血氧测定一般是通过脉搏血氧饱和度仪的指套传感器来测定,但是指套传感器在测量外周循环障碍的患者时会出现明显偏差,针对这一问题,来自西澳大利亚科廷大学物理治疗学院的Kylie Hill等进行了一项前沿性分析研究,该研究结果发表在2013年5月27日呼吸系统疾病(Respirology)杂志上。该研究结果表明一种新的脉搏血氧饱和仪传感器,前额传感器的测量结果更加接近动脉血血氧水平。
该研究组抽取了COPD患者活动后动脉化毛细血管血液样本并测定其氧合血红蛋白饱和度水平,将其分别与脉搏血氧饱和度仪指套传感器测量的结果和前额传感器测量的结果进行对比分析。在有氧运动中,运用两个脉搏血氧饱和度仪连续测量,一个连接指套传感器,一个连接前额传感器。在有氧运动前后,通过微创的方式获取动脉化毛细血管血液样本,并测量其氧合血红蛋白饱和度。COPD患者入选标准是静息状态下 血氧饱和度<90%,运动实验时血氧饱和度下降程度>4%。当前仍吸烟的患者和临床医生建议日常生活中辅助吸氧的患者被排除在外。全组共14例,FEV1=35±10%预计值。脉搏血氧饱和度仪指套传感器组与动脉化毛细血管组氧合血红蛋白饱和度对比分析指套传感器组测试水平比动脉化毛细血管组血液样本中的水平低2%(一致性界限为3%)。脉搏血氧饱和度仪前额传感器组与动脉化毛细血管组氧合血红蛋白饱和度对比分析前额传感器组测试水平比动脉化毛细血管组血液样本中的水平高2%(一致性界限为4%)。两组对比结果具有一致性。脉搏血氧饱和度仪指套传感器组、脉搏血氧饱和度仪前额传感器组、动脉化毛细血管组3组的氧饱和度在运动实验中的变化是相似的,指套组(-7%;95%可信区间CI,-4%到-10%)。前额传感器组(-7%;95%CI,-3%到-10%),动脉化毛细血管组(-6%;95%CI,-3%到-9%)。
该研究结果表明前额传感器测定的氧饱和度较动脉化毛细血管血液样本中测定氧饱和度较高。假设动脉化毛细血管中血液的氧饱和度比动脉血中的氧饱和度稍低,那么前额传感器的测量结果更加接近于动脉血的氧饱和度。而两种传感器测量的血氧结果在运动过程中都是递减的。

Comparing finger and forehead sensors to measure oxygen saturation in people with CHRONIC OBSTRUCTIVE PULMONARY DISEASE.
BACKGROUND AND OBJECTIVE
Oxyhaemoglobin saturation of arterial blood is commonly measured using a finger sensor attached to a pulse oximeter (SpO2 ). We sought to compare SpO2 measured using finger and forehead sensors with oxyhaemoglobin saturation in arterialised capillary samples (ACSs) in people with chronic obstructive pulmonary disease (COPD) during exercise.
METHODS
During an aerobic exercise task, SpO2 was measured continuously by two pulse oximeters; one connected to a finger sensor and one connected to a forehead sensor. Before and after the task, ACSs were collected to provide a minimally invasive reference measure of oxyhaemoglobin saturation. Patients with COPD were eligible for inclusion if they desaturated when walking by > 4% from resting levels to < 90%. Current smokers and those prescribed supplemental oxygen were excluded.
RESULTS
Fourteen participants completed the study (FEV1 = 35±10% predicted). Compared with ACSs, SpO2 measured via the finger sensor was 2% lower (limit of agreement 3%) and SpO2 measured via the forehead sensor was 2% higher (limit of agreement 4%). Differences were not systematic. The change in oxygen saturation during exercise was similar between the finger sensor (-7; 95% confidence interval (CI), -4 to -10%), forehead sensor (-7; 95% CI, -3 to -10%), and ACSs (-6; 95% CI, -3 to -9%).
CONCLUSIONS
Oxygen saturation measured using the forehead sensor was higher than that measured in ACSs. Assuming that oxygen saturation in ACSs is slightly less than arterial blood, forehead sensors may yield measures more concordant with arterial blood. Both sensors detected exercise-induced desaturation.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#动脉血#
81
#传感器#
61
#血氧#
66