AJRCCM:肺动脉高压患者肺外表现--口腔微生物组和全身炎症
2021-10-25 刘少飞 MedSci原创
肺动脉高压可由多种不同疾病引起。有时也没有明确的病因(特发性)。女性发生特发性肺动脉高压的几率是男性的 2 倍,确诊时的平均年龄为 35 岁。在患有这种疾病的家族中,发现了许多遗传突变(可遗传)。

肺动脉高压可由多种不同疾病引起。有时也没有明确的病因(特发性)。女性发生特发性肺动脉高压的几率是男性的 2 倍,确诊时的平均年龄为 35 岁。在患有这种疾病的家族中,发现了许多遗传突变(可遗传)。这些遗传基因突变引起肺动脉高压的实际机制尚不清楚。许多药物和毒素被发现是肺动脉高压的危险因素,如芬氟拉明(以及其他相关的减肥药物)、苯丙胺类、可卡因和选择性 5-羟色胺再摄取抑制剂 (SSRI)。
肺动脉高压患者中口腔微生物和全身炎症是怎么样的呢?
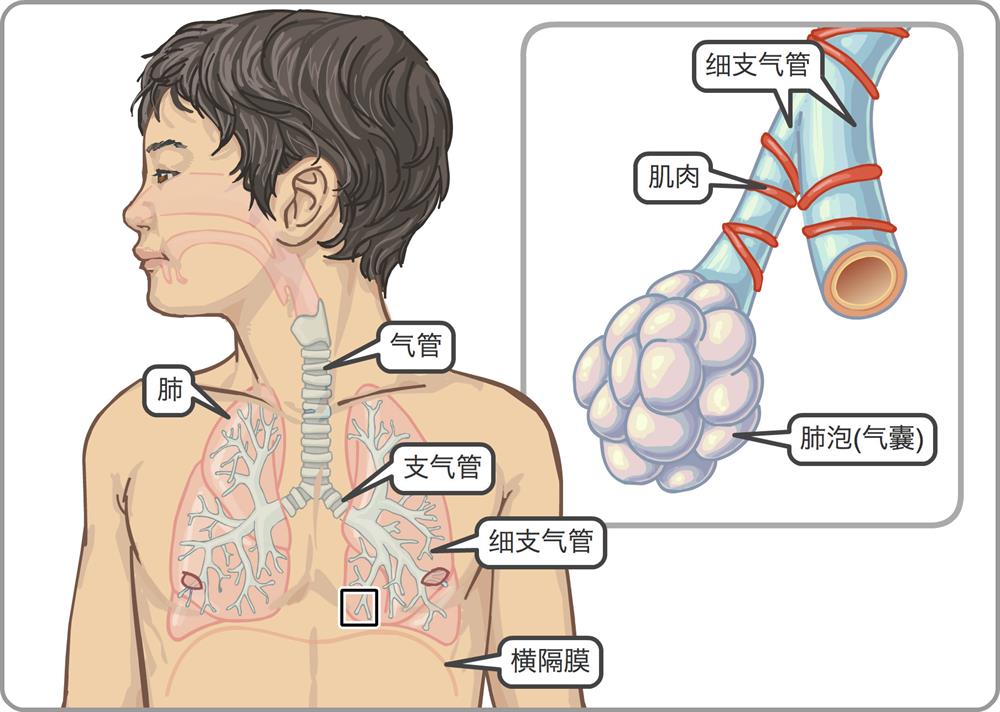
肺血管炎症已被认为是 PAH 的关键事件。尽管有证据表明血管病变内会产生促炎细胞因子,但PAH 患者的循环炎症蛋白浓度也升高,这表明炎症信号也可能来自体循环。全身性炎症可由细菌易位或细菌副产物从胃肠道进入体循环引起。最近的一项研究表明,PAH 患者与巨噬细胞活化标志物(如可溶性 CD14 [分化簇 14] 和 Toll 样受体 4)和循环 LPS 浓度具有高度相关性,表明慢性细菌易位。有趣的是,在开始 PAH 靶向治疗和改善右侧血流动力学后,循环 LPS 负荷降低,强调了右心血流动力学在肠道充血和肠道屏障功能中的重要性。需要未来的临床研究来证实这些产生假设的发现。
除了促炎特性外,共生的人类微生物组还可以通过改变 NO 和硫化氢信号传导和产生来影响肺血管平滑肌松弛和增殖。摄入的硝酸盐经过酶促和非酶促反应产生 NO,NO 在近端胃肠道迅速吸收并全身循环,从而引发有益的 NO 信号反应。大量研究表明,完整、可行的口腔微生物组对于增强内皮功能障碍和炎症的剂量依赖性改善是必要的。虽然需要进行更多的研究,但认为针对微生物组的药物干预可能在 PAH 治疗中发挥作用是很有吸引力的。
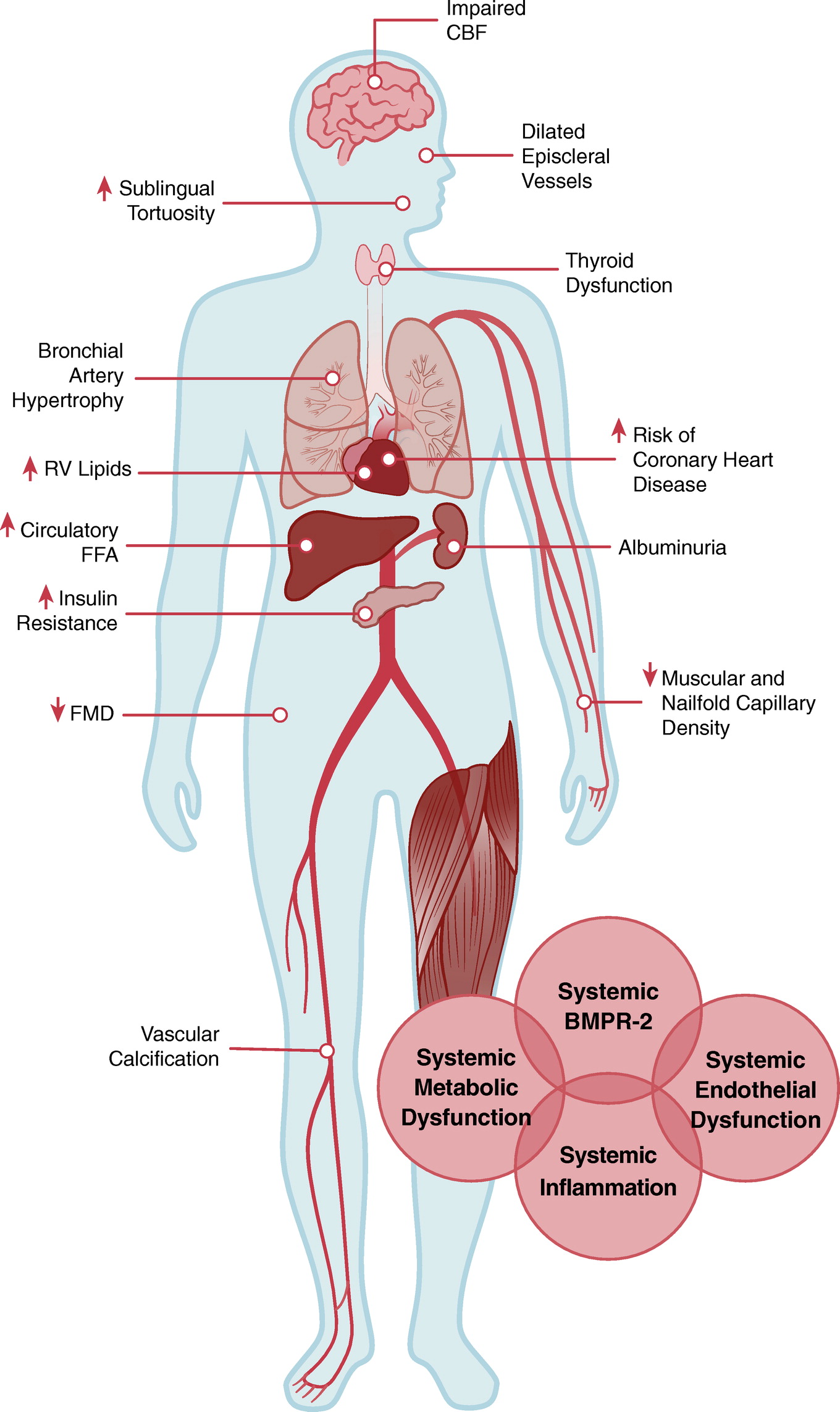
全身血管的异常血管反应和形态变化是 PAH 临床表现的一部分,会对这些患者的功能状态产生不利影响。 PAH 是一种肺部疾病,其全身表现是由多种因素引起的,包括异常的内皮反应、代谢失调和炎症。
尽管 PAH 的肺外表现在临床上通常很微妙,但它们可能会对患者的预后产生重大影响。 未来的研究可能会更多地揭示 PAH 肺外发病率的分子基础,并导致量身定制的干预措施。 在此之前,结构化的体育锻炼和控制可改变的心血管危险因素将是治疗 PAH 的重要措施。
参考文献:
Nickel NP, Yuan K, Dorfmuller P, Provencher S, Lai YC, Bonnet S, Austin ED, Koch CD, Morris A, Perros F, Montani D, Zamanian RT, de Jesus Perez VA. Beyond the Lungs: Systemic Manifestations of Pulmonary Arterial Hypertension. Am J Respir Crit Care Med. 2020 Jan 15;201(2):148-157. doi: 10.1164/rccm.201903-0656CI. PMID: 31513751; PMCID: PMC6961748.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉高压#
58
#肺动脉高压患者#
91
#RCC#
67
#微生物#
56
#微生物组#
73
#全身炎症#
63