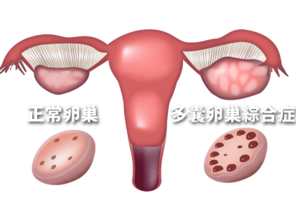
JCEM:双侧肾上腺增生可能是PCOS女性雄激素增多的原因
2016-07-06 MedSci MedSci原创
根据最新的研究表明,一些患有多囊卵巢综合征的女性,在使用地塞米松后出现了肾上腺体积变小和类固醇激素分泌增多。
根据最新的研究表明,一些患有多囊卵巢综合征的女性,在使用地塞米松后出现了肾上腺体积变小和类固醇激素分泌增多。
“一组PCOS的女性患者产生了更多的类固醇激素,同时肾上腺出现了小结节样肾上腺增生的特征”,乔治敦大学医院的华盛顿特区儿科内分泌学助理教授Evgenia Gourgari博士说道,“我们的研究表明在PCOS女性亚组中,肾上腺异常可能是此类患者出现以上症状的潜在原因”。
Gourgari和同事研究了38名患有PCOS女性,和20个健康人群作为对照,平均年龄16-19岁,评估垂体一肾上腺轴和口服小剂量及大剂量地塞米松抑制试验。主要终点包括在服用小剂量和大剂量地塞米松后尿皮质醇和17羟类固醇含量,以及CT评估的肾上腺体积。在第一天检测尿液(基线),第2和第3天每隔6小时给予口服小剂量地塞米松0.5mg,第4、5天给予口服地塞米松2mg,最后在第6天收集尿液。
结果,使用小剂量地塞米松治疗时,两组间基线和终点时尿游离皮质醇含量相似。在第6天,对照组尿游离皮质醇含量偏低(1.5 µg/m2/day) ,PCOS组 (2 µg/m2/day; P = .038),表明使用大剂量地塞米松时PCOS组与对照组相比尿皮质醇受到轻度抑制。
肾上腺体积与17-hydroxy类固醇负相关(P = .009)和尿皮质醇在5天(P <措施)。大剂量地塞米松后,被发现在肾上腺总量较小PCOS组的第75个百分位尿皮质醇和/或自由17-hydroxy类固醇(n = 15)与其余的PCOS组(n = 22;P = .003),但是没有差异雄激素过多症的胰岛素抵抗。
在第5天,肾上腺体积与17-羟类固醇(P = .009)及尿游离皮质醇负相关(P < .001)。在使用大剂量地塞米松后,PCOS组部分人群较另一部分人群(n = 22; P = .003)出现了一个整体肾上腺体积变小,大约在第75百分位的尿游离皮质醇和/或17羟类固醇(n = 15) ,但没有雄激素增多的胰岛素抵抗差异。
Gourgari说道,“PCOS亚组中的女性可能出生就伴随肾上腺的问题”。Amber Cox评价道:“这是这个领域新的观点,需要进一步证实,但是它至少能说明这个复杂和多因素疾病的部分原因,可能引领新的治疗方法。未来需要更大样本的PCOS患者来证实我们的发现,检测是否提高肾上腺激素的方法同时可以改善PCOS的症状。”
原始出处:
Adrenal volumes reduced, steroid hormone secretion increased after dexamethasone in PCOS,healio,2016
E. Gourgari1,2, M. Lodish1, M. Keil1,*, N. Sinaii3,etal,Bilateral adrenal hyperplasia as a possible mechanism for hyperandrogenism in women with polycystic ovary syndrome,JCEM,June,17 2016
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JCEM#
56
文章很好,非常有益
75
感谢分享,学习新知识了
85
#肾上腺#
66
#JCE#
62
#双侧#
50