罕见的原发低度恶性骨肿瘤1例
2017-12-19 牛晓辉 郝林 骨肿瘤
造釉细胞瘤是一种罕见的、原发低度恶性肿瘤,好发于胫骨和腓骨。好发年龄为20~50岁,男多于女。在临床上表现是什么?影像学特征又是什么?以下误诊误治病例,或许能给您启发——
造釉细胞瘤是一种罕见的、原发低度恶性肿瘤,好发于胫骨和腓骨。好发年龄为20~50岁,男多于女。在临床上表现是什么?影像学特征又是什么?以下误诊误治病例,或许能给您启发——
(1)病例介绍
:患者,女,21岁,因无明显诱因出现左小腿下端疼痛16个月,左小腿再次疼痛1周而入院。患者于16个月前无明显诱因出现左小腿下端内侧疼痛伴肿胀,无夜间痛,活动无受限,未予诊治。1年前就诊于北京某医院,摄片后考虑“纤维异样增殖症”行病灶刮除异体骨松质植骨术,术后病理回报为“造釉细胞瘤”。1周前出现左小腿下端疼痛,复查摄片示左胫骨下端溶骨区,考虑为复发,为进一步诊治而收入院。

图18‐1 X 线片示左胫骨干皮质的一溶骨性骨破坏,腓骨下段增粗,髓腔内骨破坏
入院查体:左小腿下端内侧可见约10cm 纵行手术瘢痕,左小腿下端前方有压痛,余未见异常。
化验室检查未见异常。
影像学检查:第一次术前X 线示左胫骨骨干下段皮质内的一个溶骨性破坏,皮质膨胀,基质均匀,边界清楚,皮质未见破坏,无骨膜反应及软组织包块。腓骨骨干下端髓腔内可见溶骨性破坏,皮质膨胀,无皮质破坏。如图18‐1 所示。复发时的X 线示胫骨有一溶骨性破坏。CT 示胫腓骨骨干下段溶骨性破坏,有明显的强化(图18‐2a,图18‐2b),ECT 示胫骨腓骨下段核素浓聚。
手术方案:左胫腓骨下段肿瘤截除,胫骨异体骨植入,带锁髓内针内固定术。手术经过为胫骨下段内侧切口,梭形切除原手术瘢痕,显露胫骨前内外侧面,切开胫骨前肌,显露出胫骨下段,距内踝尖5cm处,截断胫骨。再向上11cm处,再次截断胫骨。断端髓腔正常,完整地切除瘤段。用已加工好的同种异体骨行骨缺损处植骨,然后用带锁髓内针内固定。另行腓骨外侧切口,完整地切除腓骨下段肿瘤。下胫腓关节用一枚螺钉固定。

图18‐2 a﹒术后1年的X 线片示左胫骨干手术部位可见骨破坏区,考虑为复发。而未手术的腓骨干骨破坏无变化;b﹒复发时的CT 示胫骨及腓骨干溶骨性骨破坏
术后病理结果:胫骨为造釉细胞瘤,腓骨病理为纤维异样增殖症(图18‐3a,图18‐3b)。
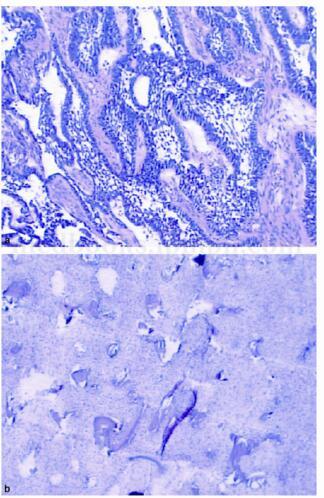
图18‐3 a﹒左胫骨典型的造釉细胞瘤病理表现;b﹒左腓骨干标本呈纤维结构不良的病理表现
(2)诊断要点
:在临床方面,造釉细胞瘤是一种罕见的、原发低度恶性肿瘤,好发于胫骨和腓骨。好发年龄为20~50岁,男多于女。造釉细胞瘤为发生于皮质的低度恶性肿瘤,约15%的患者死于转移。在临床上表现为局部的隐痛,逐渐肿胀,并出现小腿畸形。部分患者可有外伤史,晚期或复发的病变有软组织肿块。
在影像学方面,X 线表现为边界清楚、大小不等、早期孤立的放射性透亮区,逐渐长大融合成长形的多发溶骨缺损区,这些病灶被硬化的骨质隔开,可呈肥皂泡样表现。锯齿状的皮质破坏,是此病的特征。早期仅侵及前方皮质,后期逐渐长大并出现胫骨畸形。80%的病灶长度大于5cm。病灶可以膨胀和破坏皮质,形成软组织肿块。CT 平扫可看到骨破坏的细节,加强CT 可见病灶强化。ECT 示病变区同位素摄取增高。MRI 示T 1加权像为低信号,T 2加权像为高信号,在压脂像上病变信号强度不减弱。
在组织学方面,有两种不同的成分:一种为由鳞状细胞和上皮珠组成的上皮起源成分;另一种为由幼稚间叶细胞和发育不良的骨样组织组成的间叶起源成分。上皮成分由圆形到卵圆形细胞组成,有四种形态:梭形细胞型、基底细胞型、鳞状细胞型和腺样结构型,在同一肿瘤中可以含有一种或几种形态。间叶基质成分由幼稚的生成少许胶原的梭形细胞和其生成的少许胶原疏松排列,细胞大小和形态不一,星形细胞核极似纤维异样增殖症基质细胞的细胞核。纤维区域似纤维异样增殖症,但没有纤维异样增殖症中幼稚且发育异常的骨小梁。
(3)专家分析
:在影像学方面,造釉细胞瘤应与纤维结构不良、骨性纤维结构不良等鉴别。纤维结构不良为髓腔起病的瘤样病变,无侵袭性的表现,无皮质的溶骨性破坏表现。骨性纤维结构不良是一种婴幼期起病的病变,而造釉细胞瘤成人发病。
在组织学方面,造釉细胞瘤的间叶起源成分极似纤维异样增殖症,以至有人认为造釉细胞瘤是纤维异样增殖症的一种恶性亚型,但造釉细胞瘤的特有的上皮成分可以很容易与纤维异样增殖症鉴别。
(4)治疗原则
:造釉细胞瘤是一种低度恶性的原发恶性骨肿瘤,按Enneking 分期属于Ⅰb 期肿瘤,应行局部切除,达到广泛的切缘。本例患者第1次手术行囊内刮除术,术后1年复发。而第2次手术时达到广泛切除,随访7年无复发。对于早期的Ⅰa 期肿瘤,若病灶仅限于前方皮质,未侵及髓腔,大块切除后不造成节段性缺损,但是节段性切除是更明智之选。本例患者在功能重建方面,行大段异体骨移植髓内针内固定术,下胫腓关节螺丝钉内固定术,术后患者功能良好。造釉细胞瘤对放疗和化疗不敏感。

图18‐4 a﹒术后7年的侧位X 线片,异体骨已愈合,肿瘤无复发;b﹒术后7年的正位X 线片,异体骨已愈合,肿瘤无复发
(5)经验教训
:在诊断方面,造釉细胞瘤是起源于骨密质干的低度恶性肉瘤,好发于胫骨,尤其是前方皮质。应与骨性纤维结构不良、骨纤维异样增殖症等鉴别。本例患者第1次术前仅根据影像学诊断为骨纤维异样增殖症,而未行术前活检。直接行病灶刮除术,术后病理报告为造釉细胞瘤。从而导致误诊误治。第2次手术时,腓骨肿瘤被直接诊断为造釉细胞瘤,而未行活检术。术后病理报告为骨纤维异样增殖症。因此骨肿瘤的诊断原则为临床、影像、病理三结合。本例患者术前未行组织学检查,而导致误诊的出现。胫骨的造釉细胞瘤合并腓骨的纤维异样增殖症已有报道。
在治疗方面,由于造釉细胞瘤好发于胫骨骨干,行瘤段截除异体骨移植内固定术。异体骨与宿主骨的愈合多在6个月左右。可保留膝关节和踝关节,患肢功能良好。本例患者异体骨与宿主骨约6个月时愈合,腓骨肿物切除后,下端腓骨仅剩余5cm,因此行下胫腓关节螺钉内固定术,从而保持了踝穴的稳定,踝关节功能良好。
(6)随访结果
:术后每3个月定期复查,术后6个月骨愈合,无肺转移。已术后随访7年,无肿瘤复发,功能良好(图18‐4a,图18‐4b)。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了.....
102
学习了.......
138
学习了.....
115
学习了.....
109
学习了.......
88
学习了......
57
#罕见#
70
学习了......
52
学习了......
68