通过病例分享TIPS肝硬化门静脉血栓患者的治疗经验
2013-07-27 第四军医大学西京消化病医院 韩国宏 何创业 中国医学论坛报
概述 肝硬化门静脉高压是形成门静脉血栓的主要原因之一,约24%~32%的门静脉血栓患者存在肝硬化血栓形成。血栓形成可减少流向肝脏的血液量,加重肝损害。门静脉压升高可引起出血、腹水、淤血性肠坏死,甚至可导致门静脉高压性胆管病和儿童发育迟缓。 目前研究表明,门静脉血栓形成可能与门静脉阻力增加,血流状态改变有关。最新研究证实,血栓形成与患者的肝功能密切
概述
肝硬化门静脉高压是形成门静脉血栓的主要原因之一,约24%~32%的门静脉血栓患者存在肝硬化血栓形成。血栓形成可减少流向肝脏的血液量,加重肝损害。门静脉压升高可引起出血、腹水、淤血性肠坏死,甚至可导致门静脉高压性胆管病和儿童发育迟缓。
目前研究表明,门静脉血栓形成可能与门静脉阻力增加,血流状态改变有关。最新研究证实,血栓形成与患者的肝功能密切相关。
门静脉血栓的治疗方法包括:① 抗凝,低分子量肝素(LMWH)和(或)维生素K拮抗剂(VKA);② 经颈静脉肝内门体分流术(TIPS);③ 管腔内溶栓。
对于部分血栓形成患者,抗凝等内科治疗可能会有一定作用;但对于完全血栓或伴有门静脉海绵样变性的患者,内、外科治疗的效果均不会太好。特别是,对于血栓形成合并肠坏死穿孔的患者,外科治疗可能引起短肠综合征。即便切除后所剩肠道能够满足分泌及吸收功能,也无法有效改善门静脉血栓,而且术后很可能发生肠道淤血及再坏死、穿孔。
对于已接受外科干预但门静脉血栓仍然存在的患者,目前还没有特殊的后期序贯疗法。这类患者多数伴有静脉曲张出血或既往出血史,因此抗凝、溶栓治疗的风险较大。
近年来,随着TIPS技术的不断成熟和广泛应用,国内外学者已接受并采用这种技术治疗门静脉血栓。TIPS不仅可开通闭塞的门静脉血栓,还能有效解决门脉高压。
病例1
39岁男性,因“持续性腹部绞痛伴黑便2天”入院。
查体:腹平,未见肠型及蠕动波,腹肌韧,左侧腹部压痛、反跳痛明显,腹水征(+),肠鸣音减弱。既往乙肝病史,10个月前发生1次静脉曲张出血,经保守治疗缓解,于7个月前接受脾切除术。肝脏CT:肝硬化、脾切除术后、门静脉及肠系膜上静脉部分血栓形成、少量腹水。血常规:WBC 28.35×109/L,RBC 3.72×1012/L,HGB 77 g/L,PLT 114×10 9/L;肝功能:ALT 21 U/L,AST 31 U/L,ALB 29.5 g/L,TBIL 18.5 μmol/L,Child-pugh B级(9分);肾功能:BUN 11.6 mmol/L,CRE 122 μmol/L;Na+ 137.6 mmol/L,K+ 4.6 mmol/L;血凝:PT 21.3秒,APTT 46.9秒,INR 1.88,AT 43%。
行腹腔镜探查及肠切除、肠吻合术。术中见腹腔内有血性腹水,约700 ml,肝脏体积缩小,可见结节形成;距屈氏韧带50 cm起,长约70 cm的小肠颜色发黑,无蠕动及血运,其后约40 cm的肠段颜色发紫,血运差,剩余3.3 m的小肠及结肠未见异常;切除血运障碍段小肠及两端各10 cm血运正常的肠管后,行小肠端端吻合术。
术后患者消化道出血停止,但腹痛渐重,腹胀仍明显,引流出淡红色液体约1000 ml。血常规: WBC 32.84×109/L, RBC 4.26×1012/L,HGB 100 g/L,PLT 147×109/L。鉴于尚未消除患者的门静脉及肠系膜上静脉血栓,门静脉系血流阻力增加,因此肠管淤血仍然存在。
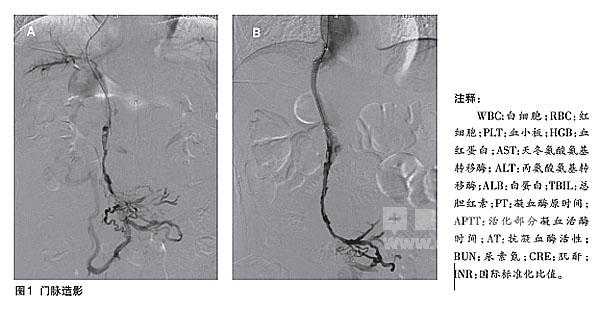
患者在肠切除术后9天腹痛加重。血常规:WBC 17.63×109/L, RBC 4.08×1012/L,HGB 99 g/L,PLT 182×109/L;肝功能:ALT 20 U/L,AST 27 U/L,ALB 30.7 g/L,TBIL 12.6 μmol/L;血凝:PT 17.2秒,APTT 63秒,INR 1.43,AT 60%;Na+ 137.4 mmol/L,K+ 4.1 mmol/L。直接门脉造影示肠系膜及门静脉主干分支造影剂充盈缺损,血流缓慢(图1A),遂行TIPS。TIPS术前门静脉压为39 cmH20,术后降至24 cmH20,门脉造影示肠系膜造影剂充盈缺损,支架血流通畅(图1B)。
术后次日,患者腹痛减轻,食欲好转;术后1周,腹痛消失。血常规:WBC 5.23×109/L, HGB 95 g/L,RBC 4.03×1012/L,PLT 383×109/L。术后20个月,患者无腹痛及复发性出血,生存状况良好。
病例2
40岁男性,因“部分肠切除术后20个月,反复呕血、黑便13个月”入院。患者因门静脉肠系膜上静脉血栓形成伴肠坏死,于20个月前行坏死部分肠段切除术及肠吻合术。此后,患者接受经皮穿刺门静脉造影+溶栓导管置入术,术后接受导管溶栓治疗。术中见肝内门静脉显影可,门静脉主干闭塞,肠系膜上静脉血管变细、扭曲,可见侧支循环建立。抗凝、溶栓治疗5天效果不佳,主干未显影。
查体:贫血貌,腹平,无肌紧张,未见肠型及蠕动波,腹软,无明显压痛及反跳痛,腹水征(-),肠鸣音正常。
血常规:WBC 2.78×109/L, RBC 3.43×1012/L,HGB 77 g/L,PLT 62×109;肝功能:ALT 15 U/L,AST 17 U/L,ALB 36.2 g/L,TBIL 12.3 μmol/L; Na+ 143.1 mmol/L,K+ 3.2 mmol/L; PT 20.3秒,APTT 57.1秒,INR 1.73,AT 47%。
CT检查:肝硬化、门静脉海绵样变性、肠系膜上静脉血栓形成、脾大。
诊断:门静脉海绵样变性、乙肝后肝硬化失代偿期、食管静脉曲张出血。
行经皮门静脉穿刺和直接门静脉造影:肠系膜上静脉血管变细、扭曲,门静脉主干未显影,可见海绵样侧支循环形成,遂行TIPS。术后造影显示支架血流通畅,血流速度加快。患者术后精神好转,食欲明显增加。
TIPS术后11个月,患者未再出现腹痛及静脉曲张出血,生存状况良好。WBC 3.02×109/L, RBC 4.24×1012/L,HGB 93 g/L,PLT 64×109/L。
结论 TIPS安全可行
对于肝硬化门静脉血栓患者,应尽早诊断,并及时对新鲜血栓予以抗凝治疗。对于完全血栓形成的患者,应早期行TIPS治疗,其目的是开通并恢复门脉血流,防止血栓进一步蔓延,这可能是成功治疗门静脉血栓的关键。
抗凝、溶栓治疗有可能增加患者的出血风险,但总体上利大于弊。
TIPS在建立门腔分流后,可降低门静脉压,有效开通堵塞的门静脉,因此能够有效防治食管胃底静脉曲张。门静脉血流速度增加,能够较好地预防门静脉血栓进一步蔓延。在血流保持通畅的情况下,通过血流冲刷作用可在一定程度上减轻门静脉血栓的程度。
笔者研究结果表明, TIPS对70%~80%的肝硬化门静脉血栓患者安全、可行。
超声引导下的经皮经肝穿刺门静脉及门静脉预成型术,可提高TIPS成功率,但可能有经皮穿刺道的出血风险,须在有经验的超声医师配合下完成。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#静脉血#
78
#TIPS#
75
#静脉#
79
#iPS#
70
#门静脉#
90