Nature Genetics:陈赛娟陈竺赵维莅等发现淋巴瘤精准治疗潜在靶点
2015-07-27 佚名 中国科学报
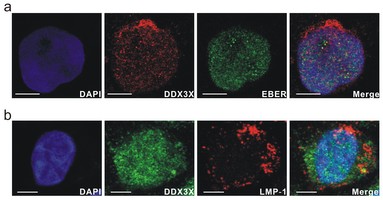
上海交通大学系统生物医学协同创新中心的上海血液学研究所联合我国血液/肿瘤临床多中心研究机构的17家医院,对/T细胞淋巴瘤(NKTCL)这一具有独特地域性和临床特征的血液肿瘤进行了基因组学、分子病理学和临床预后相关性研究,取得了精准医学领域的突破性成果。相关研究7月20日在《自然—遗传学》杂志上发表。自然杀伤/T细胞淋巴瘤是一种恶性增殖的特殊类型淋巴瘤。该病在亚洲地区人群中相对高发,发病凶险,预后很
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Genetics#
66
#Gene#
55
这篇文章有一定深度
186
是一篇不错的文章
146
厉害,
133
牛人,
163
牛人,
130
天才,赞一个!
116
天才,赞一个!
75
厉害,
144