中国进行性核上性麻痹临床诊断标准
2016-10-11 中华医学会神经病学分会帕金森病及运动障碍学组 中国医师协会神经内科医师分会帕金森病及运动障碍专业委员会 《中华神经医学杂志》2016年第4期
进行性核上性麻痹(progressive supranuclear palsy,PSP)是一种较为常见的非典型帕金森综合征,文献报道日本的患病率为2~17/10万,高于欧美的3.1~6.5/10万的患病率[1],而我国目前尚无确切的流行病学资料。PSP的发病年龄一般为50~70岁,平均病程为5~9年[2,3],特征性的临床表现为垂直性核上性眼肌麻痹伴姿势不稳易跌倒。但近年来以病理诊断为基础的病
进行性核上性麻痹(progressive supranuclear palsy,PSP)是一种较为常见的非典型帕金森综合征,文献报道日本的患病率为2~17/10万,高于欧美的3.1~6.5/10万的患病率[1],而我国目前尚无确切的流行病学资料。PSP的发病年龄一般为50~70岁,平均病程为5~9年[2,3],特征性的临床表现为垂直性核上性眼肌麻痹伴姿势不稳易跌倒。但近年来以病理诊断为基础的病例研究结果显示,PSP的临床表现变异较大,其中典型PSP(Richardson's syndrome)约占2/3,其他则早期以帕金森综合征、纯少动伴冻结步态、皮质基底节综合征、非流利性变异型原发性进行性失语、额颞叶功能障碍和小脑型共济失调等为主要临床表现,易被误诊为帕金森病(Parkinson's disease)及其他神经变性病:如多系统萎缩(multiple system atrophy, MSA)、皮质基底节变性(corticobasal degeneration, CBD)、额颞叶痴呆(frontotemporal dementia, FTD)等[4,5]。PSP的诊断仍以病理诊断为"金标准",临床尚缺乏客观的生物学标志。随着对PSP临床表型认识的进展,包括美国国立神经系统疾病与脑卒中研究所与进行性核上性麻痹学会(NINDS-SPSP)联合推荐的诊断标准在内的多种PSP临床诊断标准[6,7],在临床应用中显现出特异度高而敏感度不足的弊端,重新定义和建立新的临床诊断标准对标化临床研究、提高疾病辨识及指导可能的神经保护治疗至关重要,而我国一直以来未建立相关的诊断标准。因此,中华医学会神经病学分会帕金森病及运动障碍学组以国内外新近的临床研究及文献综述为依据,提出并建立我国的诊断标准,以期提高PSP的临床诊断正确率,减少漏诊与误诊。
PSP的临床表型
虽然典型PSP以其特征性的临床表现具有较高的辨识度,但随着研究的深入,发现PSP的临床表现变异性很大。临床表型的多样性进一步降低了原有NINDS-SPSP诊断标准的敏感度。
一、PSP理查森型(PSP-Richardson's syndrome,PSP-RS)
1964年Steele、Richardson及Olszewski首次对PSP-RS进行了病例特征的描述,又称Richardson综合征[8]。其特征性的临床表现为垂直核上性眼肌麻痹、严重的姿势不稳伴早期跌倒、假性球麻痹、中轴性肌张力增高、对称性多巴抵抗的运动不能及认知功能障碍。其中核上性眼肌麻痹是最具有诊断价值的体征,早期表现为双眼垂直性追随动作迟缓,逐渐发展成为完全性垂直凝视麻痹。姿势不稳伴跌倒则更多见且常发生于病程1年内。但也有临床早期即出现垂直核上性眼肌麻痹,晚期甚至始终未出现姿势不稳者。PSP-RS的认知功能以额叶功能障碍为主,表现为情感淡漠、轻度去抑制,以及执行功能减退,平均病程为6~8年[7,9]。
二、PSP帕金森综合征型(PSP-Parkinsonism, PSP-P)
PSP-P脑tau蛋白病理改变的分布范围及严重程度都不如RS型患者,临床早期(2年内)很难与帕金森病鉴别,可以表现为非对称性或对称性起病、动作迟缓、肌强直甚至静止性震颤等,早期可以短暂的左旋多巴治疗有效,随访6年以上临床表现与RS型相似。Williams等[10]发现在103例经病理证实的PSP患者中,有33例(32%)为这一类型,之后的研究也证实其为PSP较常见的亚型之一,平均病程为9~12年[4,7,11]。
三、PSP纯少动伴冻结步态型(PSP-pure akinesia with gait freezing,PSP-PAGF)
PSP-PAGF早期即出现起步踌躇和冻结步态,但跌倒出现较晚,偶尔伴语音低下和"小写征"。其病程可超过13年,典型的PSP症状可能延迟至9年出现甚或缺如[12]。
四、PSP皮质基底节综合征型(PSP-corticobasal syndrome,PSP-CBS)
PSP-CBS同时具有皮质和基底节受累的表现,多为不对称的肢体肌张力增高、动作迟缓、皮质感觉缺失、肌阵挛、观念运动性失用和异己肢现象,早期临床很难将其与CBD相鉴别,后期可以出现核上性凝视麻痹和跌倒,病理符合PSP诊断,病程与RS型相当[13,14]。
五、PSP非流利性变异型原发性进行性失语(PSP-non-fluent variant primary progressive aphasia, PSP-nfvPPA)
PSP-nfvPPA临床早期表现为自发性言语欠流利、言语音律障碍、错语、语法缺失及颊面部失用,后期可以出现典型PSP症状,病理上以前额叶萎缩为主,中脑萎缩不明显[15]。
六、PSP小脑共济失调型(PSP-cerebellar ataxia, PSP-C)
PSP-C在日本较为多见,近期在美国亦有报道,以小脑性共济失调为首发及主要症状,与MSA-C相比其发病年龄更晚,更多出现跌倒和凝视麻痹,同时无自主神经异常表现[16]。
七、PSP行为变异型额颞叶痴呆(PSP-behavioral variant frontotemporal dementia, PSP-bvFTD)
在经尸检证实的PSP中[16],有5%~20%以行为异常和认知功能障碍为主要临床表现,其与FTD很难鉴别,平均病程为8年。
临床诊断标准
一、诊断所需条件
(一)纳入条件
1.隐匿起病,病程逐渐进展。
2.发病年龄≥30岁。
3.临床症状:临床症状为并列条件可以同时具有或单独存在。(1)姿势不稳:①病程第1年出现明显的反复跌倒;②1年后出现反复跌倒。(2)病程2年内出现:①垂直性核上性向下或向上扫视缓慢;②凝视麻痹。(3)病程2年后出现:①垂直性核上性向下或向上扫视缓慢;②凝视麻痹。
(二)支持条件
1.中轴性肌强直或多巴抵抗的帕金森症。
2.早期的吞咽困难或构音障碍。
3.存在额叶认知功能障碍、冻结步态、非流利性失语或假性球麻痹等无法用排除条件中所列疾病解释的临床表现。
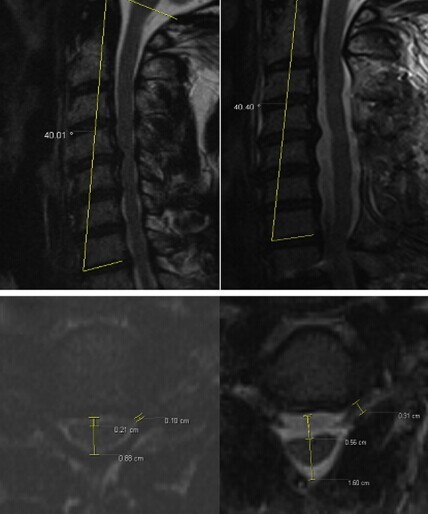
4.头颅MRI:正中矢状位T1WI MRI:(1)表现为以中脑萎缩为主的特征性征象:中脑背盖上缘平坦及蜂鸟征;(2)核磁共振帕金森综合征指数(magnetic resonance parkinsonism index,MRPI)=脑桥与中脑的面积比值×小脑中脚/小脑上脚宽度比值>13.55;(3)中脑和脑桥长轴的垂直线比值<0.52或中脑长轴垂直线<9.35 mm。
5.嗅觉检查和心脏间碘苄胍(MIBG)闪烁显像正常。
(三)排除条件
1.有其他帕金森综合征病史。
2.与多巴胺能药物无关的幻觉和妄想。
3.严重不对称性帕金森症。
4.采用多巴胺受体阻滞剂或多巴胺耗竭剂治疗,且剂量和时间过程与药物诱导的帕金森综合征一致。
5.神经影像学有结构损害的依据(如基底核或脑干梗死、占位性病变等)。
6.阿尔茨海默型皮质性痴呆。
7.局限性额叶或颞叶萎缩。
8.早期出现明显小脑共济失调。
9.早期显著的自主神经功能障碍。
二、诊断标准
(一)临床确诊的PSP-RS
必备纳入条件为1、2、3(1)①和(2)②及支持条件4中的两项;无排除条件。
(二)很可能的PSP-RS
必备纳入条件为1、2、3(1)①和(2)①及支持条件5;无排除条件。
(三)很可能的PSP-P
必备纳入条件为1、2、3(3)①或②和支持条件1、5;无排除条件。
(四)可能的PSP
必备纳入条件为1、2、3(1)②或(2)①或(3)①伴有支持条件1、2、3其中一项;无排除条件1~6。
诊断标准建立的背景与依据
一、诊断标准的框架设立
目前临床应用较为普遍的NINDS-SPSP诊断标准将PSP的诊断分为3个层面,包括病理确诊、临床很可能和临床可能的PSP。但在实际操作过程中,病理确诊在患者生前很难实现,"临床很可能标准"针对PSP-RS型的特异度和阳性预测值较高而敏感度不足,同时无法涵盖目前了解的PSP其他临床类型[6]。2008年NNIPPS(Neuroprotection and Natural History in Parkinson Plus Syndromes)建立的诊断标准在之后的临床应用中,无论其敏感度、特异度和阳性预测值均未超过NINDS-SPSP的诊断标准[17]。本标准以上述2个标准为基本框架,依据国际上新近的PSP临床表型和与诊断相关的生物学标志,尽量提高应用本标准诊断疾病的特异度和敏感度。由于PSP的临床异质性,标准越精确,其敏感度必然降低。因此,我们将标准的疾病诊断条件分为纳入条件、支持条件和排除条件3部分,依据患者具备的条件将诊断分为临床确诊的PSP-RS、很可能的PSP-RS及PSP-P、可能的PSP。
二、诊断所需条件的设立
纳入条件为疾病的特征性表现,包括病程为隐匿起病逐渐进展;发病年龄多在40岁以上,也有报道30岁以后发病,NINDS-SPSP诊断标准[6]应用≥40岁为年龄界定,研究证实典型PSP均大于此年龄发病,NNIPPS标准[17]采用年龄≥30岁,我国一项纳入103例病例的研究中确有2例患者年龄在30~40岁之间[3],因此,标准将后者作为年龄界定更为合适。在纳入条件中的临床症状部分,仍以典型的PSP表现即垂直性核上性凝视麻痹和姿势不稳伴跌倒为主,仅就跌倒年限进行了分层,临床确诊的典型类型1年内出现跌倒,相关研究显示多数很可能PSP患者出现特征性的临床表现要在2年以上,且眼球运动障碍首先表现为向上或向下扫视缓慢[18]。
在既往支持条件的基础上,我们加入了近年来做过PSP诊断和鉴别诊断相关特异度和敏感度研究的生物学标志作为支持条件,可以更加客观地帮助建立临床诊断分层。由于越来越多的研究提示以典型症状发病的PSP患者仅占病理确诊患者的少部分,有近1/3的患者是以帕金森症起病,其他不典型PSP早期症状各异,因此,将帕金森症症状和其他不典型症状作为支持条件,以协助很可能和可能病例的诊断[7,11,12,13,14,15,16,17,18,19],可以增加本标准对疾病诊断的敏感度。近年来,对PSP最具诊断价值的生物学标志当属影像学技术,磁共振扫描技术的应用为临床确诊提供了较为可靠的理论依据。针对PSP中脑萎缩的测量方法多样,早期的研究以测量T1加权像正中矢状位中脑直径为主,中脑直径平均<13.4 mm有助于鉴别诊断[20],但研究未就其对诊断PSP的敏感度和特异度进行考证。近年来,多项研究证实MRPI对PSP诊断的敏感度和特异度优于单纯中脑/脑桥比值,当MRPI>13.55时,其特异度和敏感度甚至可高达100%[21,22,23]。2013年,欧洲神经科学协会联盟和国际运动障碍协会(EFNS/MDS)推荐正中矢状位T1WI MRI表现中脑背盖上缘平坦及蜂鸟征和小脑上脚萎缩作为帕金森病和PSP鉴别诊断的依据(A级推荐)[24]。因此,本标准当中将上述两项影像学表现作为临床确诊的支持条件。仅有一项针对病理确诊的PSP和帕金森病、MSA鉴别诊断的研究提示,当中脑直径<9.35 mm且中脑/脑桥比值<0.52时,诊断PSP的特异度高达100%,但此结果缺乏其他相关研究的进一步验证[25]。大脑脚水平轴位T1WI MRI呈现中脑前后径明显缩短或中脑被盖部外侧缘凹陷,此表象缺乏客观的数值界定。因此,标准未将此作为诊断的支持条件。影像学改变虽然具有较高的特异度,但是由于其往往出现在疾病的中晚期,并不适合作为疾病早期诊断的必备条件。在支持条件中加入嗅觉检查和心脏MIBG闪烁显像,一方面是由于2015年MDS在关于帕金森病的诊断标准中,将嗅觉丧失或心脏MIBG闪烁显像存在心脏去交感神经支配作为帕金森病的支持诊断[26];另一方面由于近期研究显示嗅觉检查联合心脏MIBG闪烁显像鉴别帕金森病与PSP、MSA的特异度高达91%[27],病理确诊的各个临床表型的PSP患者,其心脏MIBG闪烁显像结果均为阴性[7]。
排除条件基本保留了既往国际标准的框架,强调早期显著的自主神经和小脑共济失调及额颞叶局限性萎缩仅作为临床确诊和PSP-RS型及PSP-P型很可能的排除条件。一项最新的经病理确诊为MSA、PSP、路易体痴呆及帕金森病的研究结果[5]提示,PSP患者性功能障碍、体位性低血压的发生明显少于其他疾病,但排尿困难及便秘并不少见,同时非典型PSP中存在以小脑功能障碍及FTD为主要表现的临床表型,因此,自主神经功能障碍、小脑功能障碍及局限性额颞叶萎缩不作为可能PSP的排除标准。加入药物引起的帕金森症和影像学占位性病变作为排除条件,并将可作为排除因素的相关临床表现进行拆分,借鉴了最新的帕金森病、CBD及MSA的相关诊断标准[13,26,28]。
三、诊断标准及分层
利用上述纳入条件、支持条件和排除条件进行疾病诊断,标准中设立了临床确诊的PSP-RS(经典型PSP),即在NINDS-SPSP很可能PSP诊断标准中加入了具有高特异度的影像学条件,符合目前对于PSP-RS的临床认识,以最大限度地提高诊断的特异度。典型PSP的很可能诊断标准基本沿用了NINDS-SPSP很可能诊断标准,仅在临床症状的描述和排除条件上略有改变。通过对PSP临床表型的深入了解,建立PSP-P型的很可能诊断标准对于疾病鉴别诊断的意义重大,此项标准是基于最新的临床研究及相关疾病的诊断标准建立的,尽量平衡了临床应用对疾病诊断的敏感度和特异度。PSP的可能诊断标准,尽量涵盖了目前所了解的PSP的各种临床表型,在扩大疾病诊断敏感度的同时,增加了相关检查的应用以避免特异度的降低。
执笔 陈海波、苏闻、陈生弟
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#进行性#
58
谢谢分享!
94
始终觉的这个难
90
#诊断标准#
51
#临床诊断#
69
#进行性核上性麻痹#
111
好赞学习分享
77
这个还是比较少见的疾病
86
学习了,赞一个!!!
82
继续关注
53