Science:科学家发现ALS和FTD等神经退行性疾病病因
2015-05-26 佚名 生物通
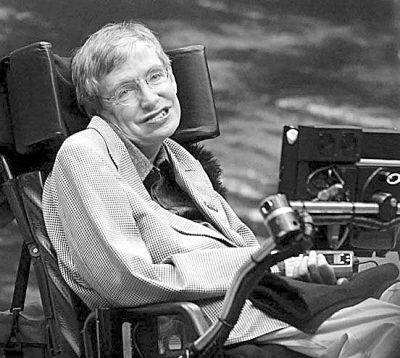
来自美国梅奥诊所(Mayo Clinic)的科学家们构建出了一种新型小鼠,其显示出与肌萎缩侧索硬化症(ALS,又称渐冻人症)和额颞痴呆(FTD)最常见的遗传形式相关的一些症状和神经退行性变。ALS和FTD这两种疾病都是由于C9ORF72基因突变引起。这项研究发布在近期的《科学》(Science)杂志上。 美国有3万多ALS患者,ALS破坏了控制包括说话、行走、呼吸和吞咽等基本动作的神
来自美国梅奥诊所(Mayo Clinic)的科学家们构建出了一种新型小鼠,其显示出与肌萎缩侧索硬化症(ALS,又称渐冻人症)和额颞痴呆(FTD)最常见的遗传形式相关的一些症状和神经退行性变。ALS和FTD这两种疾病都是由于C9ORF72基因突变引起。这项研究发布在近期的《科学》(Science)杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#科学家发现#
106
#退行性疾病#
76
#神经退行#
102
看看
169
#SCIE#
86
#FTD#
90