Nature:这么牛?单一蛋白就可引发帕金森疾病及多系统萎缩症的发生
2015-06-12 佚名 生物谷
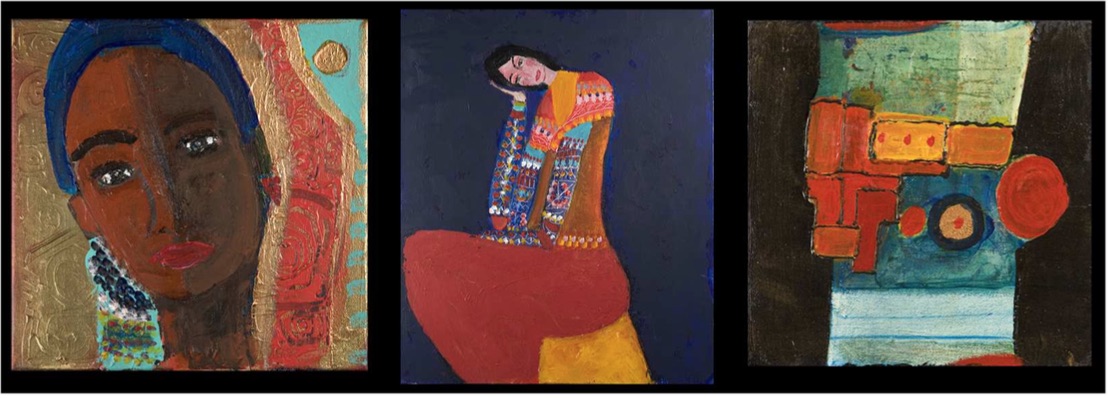
许多神经变性障碍都是由名为α-突触核蛋白的单一蛋白的集聚而引发,近日刊登在国际杂志Nature上的一篇研究论文中,来自安特卫普大学(University of Antwerp)等处的研究人员通过揭示了这些聚集物的结构及形状,同时研究者还发现这些聚集物可以决定个体是否患帕金森疾病或多系统萎缩症。典型的神经变性疾病就是大脑细胞间交流被打断同时还会引发特殊大脑区域出现细胞的缺失,对于某些大脑疾病而言这种
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












这篇文章有一定深度
141
是一篇不错的文章
163
#萎缩#
48
#Nat#
64
好好
193
看看
141
圆筒和长条的作用机制是什么呢
175
#帕金森疾病#
0
#多系统萎缩#
57
继续努力
170