Nature:一种新型干细胞--“区域选择性多能干细胞”(rsPSCs)被发现
2015-05-11 MedSci MedSci原创
一种最新发现的干细胞类型比胚胎干细胞更容易在实验室中生长。 一种最新发现的干细胞类型能帮助提供人类早期发育的模型,并且最终使人类器官在诸如猪、牛等大型动物体内得以生长,以用于研究或治疗目的。 美国加州索尔克生物研究所的发育生物学家Juan Carlos Izpisua Belmonte和他的同事在试图将人多能干细胞植入小鼠胚胎时,偶然发现了一种此前并未知晓的、可产生任何种类器官
一种最新发现的干细胞类型能帮助提供人类早期发育的模型,并且最终使人类器官在诸如猪、牛等大型动物体内得以生长,以用于研究或治疗目的。
美国加州索尔克生物研究所的发育生物学家Juan Carlos Izpisua Belmonte和他的同事在试图将人多能干细胞植入小鼠胚胎时,偶然发现了一种此前并未知晓的、可产生任何种类器官的多能细胞类型。
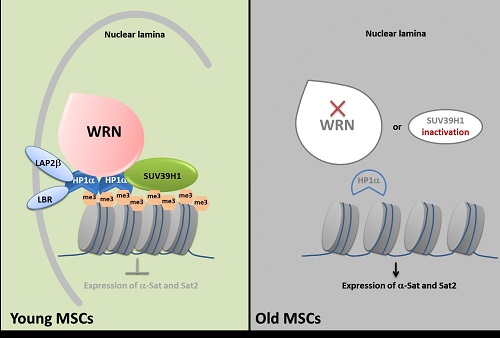
此前,科学家知道两种其他类型的多能干细胞,但让它们大量生长或引导其发育成特定类型的成年细胞被证明非常困难。在《自然》杂志上,Izpisua Belmonte及其同事报道了一种新型多能细胞。它们更容易在试管内生长,并且当被注射在合适的位置时,更容易被植入胚胎中。研究人员将其称为“区域选择性多能干细胞”(rsPSCs)。
俄亥俄州凯斯西储大学发育生物学家Paul Tesar表示,由于这些区域选择性细胞比其他多能细胞生长得更快、更稳定,因此它们在发展新的疗法方面或许更加有用。
Izpisua Belmonte和同事试图将已知类型的人类多能细胞移植到试管内的小鼠胚胎中。他们通过在含有不同组合的生长因子和化学物质的基质中培育出这些细胞。一种混合基质在使细胞生长和增殖方面表现得更加突出。研究发现,和其他多能干细胞相比,在这种溶液中发育的细胞展现出不同模式的新陈代谢和基因表达,但它们无法被很好地植入小鼠胚胎。
为找到阻止这种细胞和胚胎融合的因素,研究人员将人类细胞注入一只7.5天大的小鼠胚胎内的位置3个不同。36个小时后,只有被植入胚胎尾巴的细胞,被整合并发育成正确的细胞层,从而形成“杂交的”胚胎—— 一个DNA拥有不同起源的有机体。由于这些细胞看上去偏好胚胎中的某个部位,因此研究人员将它们称为区域选择性细胞。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#选择性#
0
#Nat#
57
#PSC#
52
很不错
131
OK
91