Clin Cancer Res:晚期食管癌采用纳武单抗二线治疗的长期预后
2022-04-07 Nebula MedSci原创
纳武单抗作为既往治疗过的晚期食管癌的二线疗法具有优于化疗的长期总生存期优势
食管癌是最具侵袭性的胃肠道癌症之一,是全球癌症相关死亡的第七大原因,2020年全球约新增6041000例食管癌。晚期食管鳞状细胞癌(ESCC)患者采用免疫检查点抑制剂治疗的长期预后信息数据有限。
ATTRACTION-3是一项随机的、多中心、开放标签的3期临床试验,本文汇报了该试验中纳武单抗 vs 化疗(紫杉醇或多西他赛)在既往接受过治疗的 ESCC 患者中的 3 年随访数据。
年满20岁的不可切除的晚期或复发性ESCC患者被随机(1:1)分成两组,接受纳武单抗或化疗(紫杉醇或多西他赛)治疗直到病情进展或不可耐受的毒性。主要终点是总生存期(从随机分组到全因死亡)。并探索了4个月时有无获得最佳缓解(BOR)与总生存期的相关性。
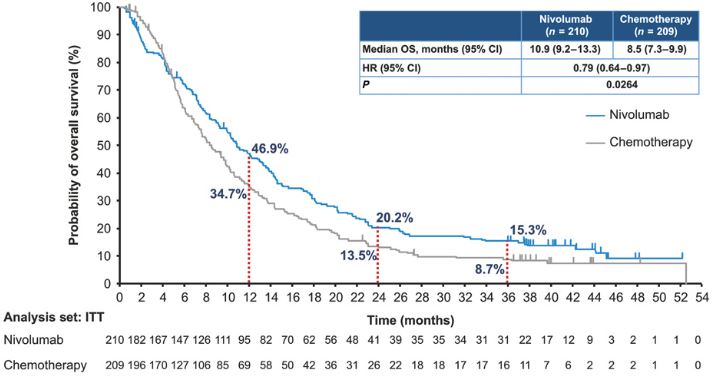
两组的总生存期
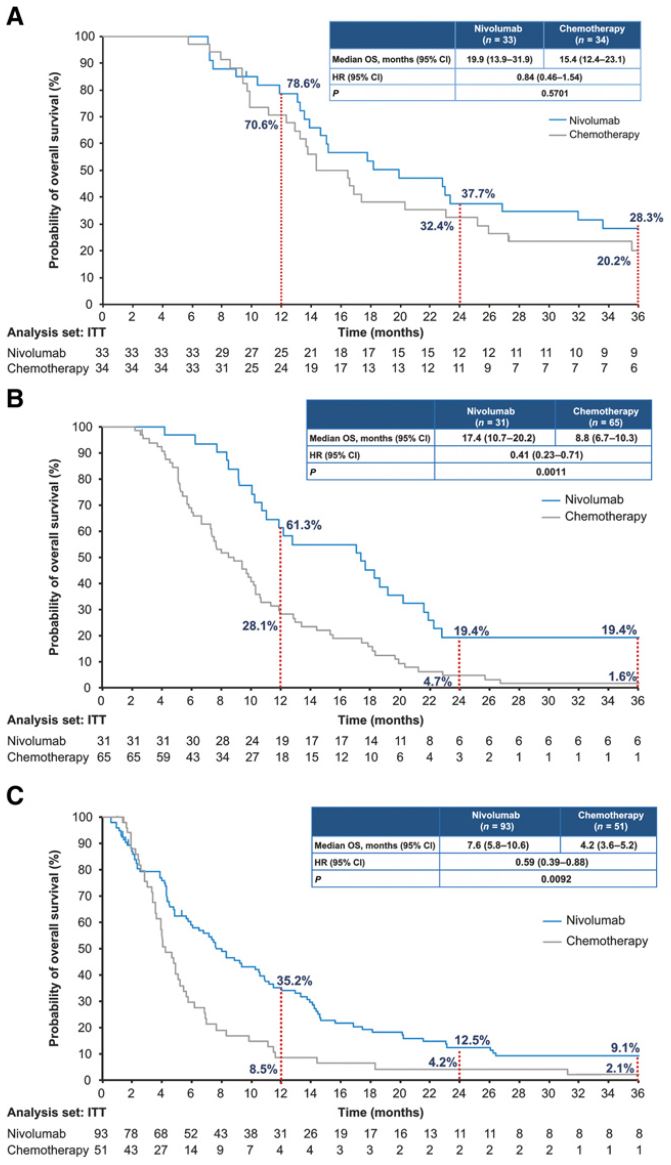
共招募了419位患者,其中210位接受了纳武单抗治疗,209位接受了化疗。最短随访了36.0个月,纳武单抗组的总生存期长于化疗组(中位总生存期:10.9个月 vs 8.5个月,HR 0.79,p=0.0264),3年总生存率分别是15.3%和和8.7%。无论有无获得最佳缓解,纳武单抗组的中位总生存期都长于化疗组(完全/不完全缓解:19.9个月 vs 15.4个月;病情稳定:17.4个月 vs 8.8个月;病情进展:7.6个月 vs 4.2个月)。
两组根据缓解情况分亚组的总生存期
纳武单抗组和化疗组分别有40位(19.1%)和133位(63.9%)患者报告了3级及以上的治疗相关的不良反应,最常见的是皮肤和胃肠道反应。
总之,该研究结果表明,纳武单抗作为既往治疗过的晚期食管癌的二线疗法具有优于化疗的长期总生存期优势。与化疗组相比,纳武单抗组的患者无论是否获得最佳缓解总生存期都有所延长,而且纳武单抗的耐受性良好。
原始出处:
Morihito Okada, et al. Three-Year Follow-Up and Response–Survival Relationship of Nivolumab in Previously Treated Patients with Advanced Esophageal Squamous Cell Carcinoma (ATTRACTION-3). Clin Cancer Res OF1–OF10. https://doi.org/10.1158/1078-0432.CCR-21-0985.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#长期预后#
83
学习
89
学习
79
学到了很多
82
#食管#
64
#二线治疗#
79
#晚期食管癌#
63