2016心脏骤停研究进展,值得一看!
2016-08-25 MedSci MedSci原创
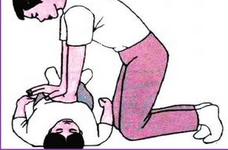
心脏骤停(cardiac arrest, CA)是全世界成人死亡的主要原因之一,每年罹患数百万人。及时有效的心肺复苏(cardiopulmonary resuscitation, CPR)是其唯一救治措施,但救治成功率低,出院存活率 <7%,神经系统损伤是其主要致死和致残原因。 心脏骤停(cardiac arrest, CA)是全世界成人死亡的主要原因之一,每年罹患数百万人。及时有效的心肺复苏
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#研究进展#
56
学习了,赞一个!!!
75
学习了,赞一个!!!
80
学习了,赞一个!!!
74
学习了,赞一个!!!
74
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
83
赞?
48
深度好文,赞一个!!!
47
深度好文,赞一个!!!
45
学习了谢谢!
38