JMCC:乳腺癌他莫昔芬耐药性可能与Snail/Slug信号有关
2014-06-26 MedSci MedSci原创
国际学术期刊Journal of Molecular Cell Biology在线发表了中国科学院上海生命科学研究院生物化学与细胞生物学研究所葛高翔研究组的最新研究成果 “Snail and Slug mediate tamoxifen resistance in breast cancer cells through activation of EGFR–ERK independen
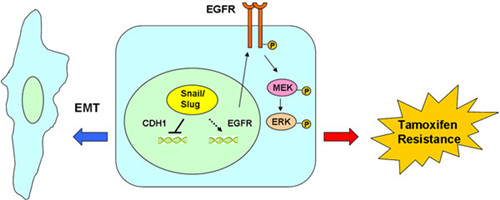
国际学术期刊Journal of Molecular Cell Biology在线发表了中国科学院上海生命科学研究院生物化学与细胞生物学研究所葛高翔研究组的最新研究成果 “Snail and Slug mediate tamoxifen resistance in breast cancer cells through activation of EGFR–ERK independent of epithelial–mesenchymal transition”。该文揭示了乳腺癌他莫昔芬耐药性产生的分子机制。
临床上,他莫昔芬是雌激素受体阳性乳腺癌病人内分泌治疗的一线药物。他莫昔芬耐药性的产生与肿瘤的复发是临床面临的重大挑战。葛高翔研究组博士研究生姜妍、赵晓彤等的研究发现,上皮-间质转化转录因子 Snail/Slug通过上调EGFR的表达并激活其下游MAPK信号通路,诱导雌激素受体阳性乳腺癌细胞产生对他莫昔芬的耐受。这一过程不依赖 Snail/Slug引起的上皮细胞间质样转化。这一研究对阐明乳腺癌他莫昔芬耐受产生的分子机理,并鉴定他莫昔芬耐药性的特征生物标志物及治疗靶位点具 有重要意义。
该项研究工作与中国科技大学朱涛研究员合作完成,得到国家科技部(蛋白质重大研究计划)、国家自然科学基金委的经费支持。
原始出处:
Jiang Y, Zhao X, Xiao Q, Liu Q, Ding K, Yu F, Zhang R, Zhu T, Ge G.Snail and Slug mediate tamoxifen resistance in breast cancer cells through activation of EGFR-ERK independent of epithelial-mesenchymal transition.J Mol Cell Biol. 2014 Jun 10. pii: mju019.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








挺好的,不错!
168
#JMCC#
67
#Snail#
64
#他莫昔芬#
57