肝纤四项的临床意义,你了解多少?
2016-05-09 佚名 检验医学网
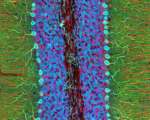
血清肝纤维化四项指标有Ⅲ型前胶原(PCⅢ)、Ⅳ型胶原(C-Ⅳ)、层粘蛋白(LN)和透明质酸(HA)。这些指标的升高常提示肝组织内的纤维化形成。肝细胞的炎性改变可以刺激肝内纤维组织增生,引起肝纤维化指标的异常。这一异常改变随着肝纤维化的程度加重而逐渐明显。这是一个由量变到质变的过程,在急性肝炎中即可见到,慢性活动性肝炎比慢性迁延性肝炎的改变更明显。Ⅲ型前胶原(PCⅢ) Ⅲ型前胶原反映肝内I
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









很不错额
116
很不错额
101
真的学习到了
58
以后多看看
58
今天材料可到
127
今天材料可到
104
肝纤维四项,临床上,检查这类比较少。
115
值得阅读,学习!
90
很久以前就开始用这个检查,到今天也几十年来,有没有什么更新
97
学习中
70