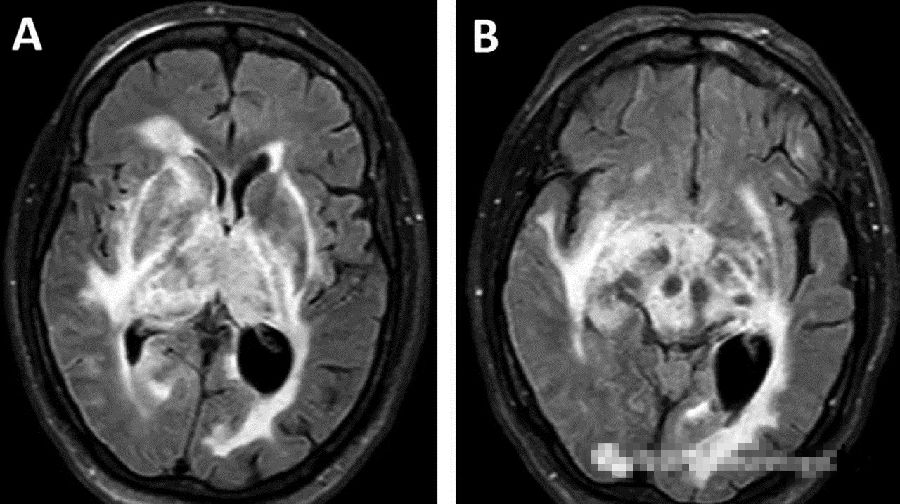
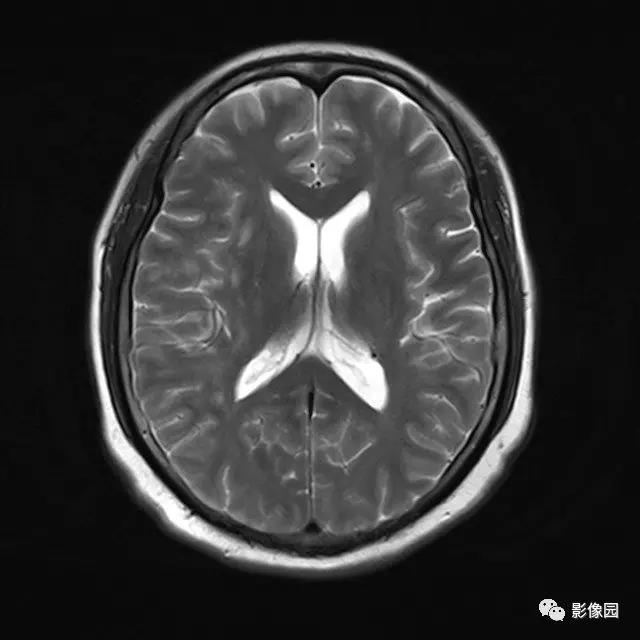
中枢神经系统铁沉积症合并椎管内肿物1例
2019-08-10 张群英 耿建红 逯冉冉 中国实用神经疾病杂志
患者,男,38岁,已婚,因“听力下降2a,大小便控制困难2a”于2017-06-08潍坊医学院附属医院脊柱外科住院。患者2a前无明显原因出现双耳耳鸣,呈阵发性,具体音调不能判别,突然仰颈时易诱发,发作时不能听清他人言语内容,自觉耳内伴有随呼吸一致的“通风声”,右耳较左耳严重,低头休息后症状逐渐缓解,每次持续时间不一,约数秒至数分钟,无眩晕、恶心、呕吐,无复视、视物模糊,无吞咽困难、饮水呛咳。后病情

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#椎管#
83
#肿物#
74
#椎管内#
100
#铁沉积#
77
#铁沉积症#
63
#神经系统#
67
#中枢神经#
0