JCO:首次完全缓解后的DLBCL病人是否需要常规影像检查?
2015-10-10 赵洲 译 MedSci原创
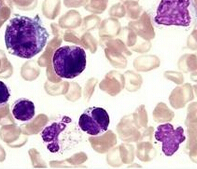
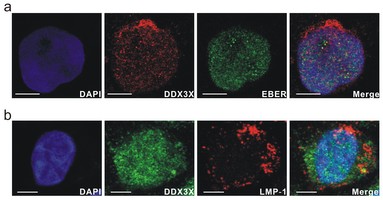
弥漫性大B细胞淋巴瘤(DLBCL)患者中有超过六成在接受联用免疫疗法和化疗的一线治疗后可以获得长期的缓解。治疗失败主要发生在病程初期。在经过一段时间的完全缓解后的DLBCL复发只出现在两成一下的经过一线疗法的获得完全缓解的病人身上。常规成像研究被常常用于临床随访从而帮助早期复发检测。尽管使用常规成像用于临床前复发检测可以获得更好的诊断结果,但是DLBCL的常规成像的实际价值是有争议的,
Tarec Christoffer El-Galaly, Lasse Hjort Jakobsen, Martin Hutchings ei al. Routine Imaging for Diffuse Large B-Cell Lymphoma in First
Complete Remission Does Not Improve Post-Treatment Survival: A Danish–Swedish Population-Based Study.JCO.October 5, 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#LBCL#
47
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
62
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
71
#完全缓解#
66
#JCO#
45
#DLBCL#
66
#影像检查#
52