Eur Urol Focus:活检格里森等级5组的模式(4+5 vs 5+4 vs 5+5)能够预测根治性前列腺切除术或外照射放疗后的生存率
2021-05-06 AlexYang MedSci原创
之前对Gleason分级组(GGG)5癌症中不同Gleason模式的癌症特异性死亡率(CSM)分析受到样本量的限制。
之前对Gleason分级组(GGG)5癌症中不同Gleason模式的癌症特异性死亡率(CSM)分析受到样本量的限制。

最近,有研究人员调查了接受根治性前列腺切除术(RP)或体外放射治疗(EBRT)的患者中,不同活检GG5模式(4+5 vs 5+4 vs 5+5)的CSM差异情况。
研究共包括了17263名符合条件的活检时患有GG 5癌症的患者(RP:n=7208;EBRT:n=10 055),其中12705名为Gleason 4+5,3302名为Gleason 5+4,1256名为Gleason 5+5疾病。研究发现,中位年龄、诊断时的前列腺特异性抗原(PSA)、晚期cT和cN阶段因Gleason模式而有明显的不同(Gleason 4+5 vs 5+4 vs 5+5;所有P<0.001)。Gleason 4+5的10年CSM率为18.2%,Gleason 5+4为28.0%,Gleason 5+5为39.1%(P<0.001)。在对整个队列的多变量分析中,调整了PSA、诊断时年龄、cT和cN阶段后,相对于Gleason 4+5,Gleason 5+4和Gleason 5+5的CSM分别高出1.6倍和2.2倍。此外,相对于Gleason 4+5,Gleason 5+4和Gleason 5+5在RP和EBRT亚组中分别与1.6和2.5倍以及1.5和2.1倍更高的CSM率相关(所有P<0.001)。
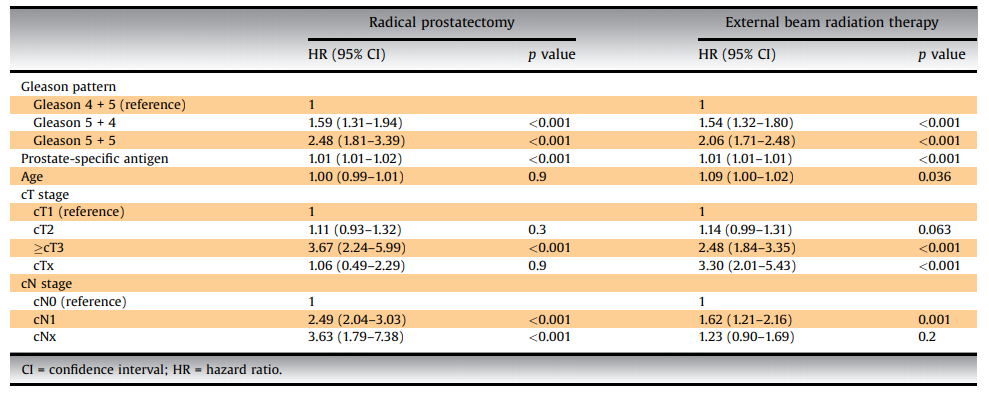
最后,研究人员指出,对于接受RP或EBRT治疗的活检GG5前列腺癌患者,Gleason模式存在重要的CSM差异(4+5 vs 5+4 vs 5+5)。理想情况下,在治疗前风险分层中应考虑个体的Gleason模式。
原始出处:
Mike Wenzel, Christoph Würnschimmel, Francesco Chierigo et al. Pattern of Biopsy Gleason Grade Group 5 (4 + 5 vs 5 + 4 vs 5 + 5) Predicts Survival After Radical Prostatectomy or External Beam Radiation Therapy. Eur Urol Focus. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#前列腺切除#
87
#切除术#
82
#生存率#
72
#活检#
89
#根治#
84