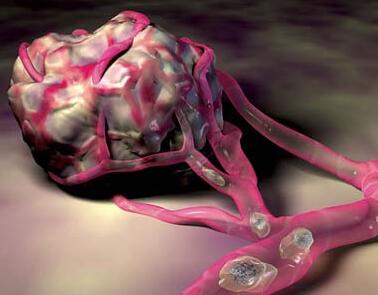
ATVB:VEGF-A调节清道夫受体BI的细胞定位及HDL跨内皮转运
2017-04-19 MedSci MedSci原创
低密度脂蛋白和高密度脂蛋白(LDL和HDL)必须通过内皮层,在血管壁内分别发挥促进和抑制动脉粥样硬化作用。然而,限制脂蛋白跨内皮转运速率的因素尚不清楚。因此,本研究用激酶药物抑制剂做高通量筛选,以鉴定跨内皮转运LDL和HDL的调节剂。用141种激酶抑制药物和荧光标记的LDL或HDL孵育人主动脉内皮细胞,继而进行基于显微镜的高通量筛选。血管内皮生长因子受体(VEGFR)的抑制剂显着抑制HDL而不是L
低密度脂蛋白和高密度脂蛋白(LDL和HDL)必须通过内皮层,在血管壁内分别发挥促进和抑制动脉粥样硬化作用。然而,限制脂蛋白跨内皮转运速率的因素尚不清楚。因此,本研究用激酶药物抑制剂做高通量筛选,以鉴定跨内皮转运LDL和HDL的调节剂。
用141种激酶抑制药物和荧光标记的LDL或HDL孵育人主动脉内皮细胞,继而进行基于显微镜的高通量筛选。血管内皮生长因子受体(VEGFR)的抑制剂显着抑制HDL而不是LDL的摄取。敲低VEGFR 2显着降低125I-HDL而不是125I-LDL的细胞结合、偶联和跨内皮转运。使用RNA干扰VEGFR1或VEGFR3并无影响。在VEGF-A缺失的细胞培养基中,HDL而非LDL的结合、摄取和转运显着降低,再给予VEGF-A可恢复这一现象。 VEGF-A对HDL的内皮结合、摄取和转运的恢复作用可被磷脂酰肌醇3激酶/蛋白激酶B或p38丝裂原活化蛋白激酶抑制,也可被清道夫受体BI敲低而消除。此外,发现VEGF-A存在是清道夫受体BI在内皮细胞质膜中定位的先决条件。
VEGF作为HDL而非LDL的跨内皮转运的调节因子,说明内皮是脂蛋白进入血管壁的特异性、可药用的屏障。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#TVB#
61
#转运#
55
#HDL#
63
#VEGF#
59
好的,科研好的发展好
91