JCEM:骨代谢标志物与牙周炎有关
2015-05-10 MedSci译 MedSci原创
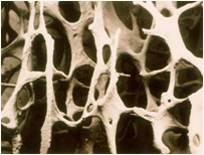
骨代谢标志物与牙周病的严重程度有关一项新的研究发现表明,一组不同的骨代谢标志物与较严重的牙周病有关。研究人员发现,患有较重牙周病的老年人血液中甲状旁腺激素(PTH)和维生素D的水平明显升高。近年来,越来越多的人关注与牙周病发生发展相关的系统性疾病,这并不意味着这些系统性疾病会导致牙周病,但是,患有这些系统性疾病的患者患在细菌引发炎症时,更易感牙周病。Dr. Schulze-Spate以及她的同事从
一项新的研究发现表明,一组不同的骨代谢标志物与较严重的牙周病有关。研究人员发现,患有较重牙周病的老年人男性(65岁以上)血液中甲状旁腺激素(PTH)和维生素D的水平明显升高。
近年来,越来越多的人关注与牙周病发生发展相关的系统性疾病,这并不意味着这些系统性疾病会导致牙周病,但是,患有这些系统性疾病的患者患在细菌引发炎症时,更易感牙周病。
Dr. Schulze-Spate以及她的同事从近6000名男性骨质疏松患者中招募了1347名患者进行了一次研究。这些研究对象分布在六个地点,对其中两个地点的65岁及以上的研究对象进行了临床评估,记录了他们的医疗和牙科病史信息,并检查了他们牙齿缺失、种植牙及牙周病的情况。对这些研究对象还进行了完整的牙周检查,基于随机检查半口的临床牙周附着丧失(CAL)、牙周袋深度、牙石、菌斑及探诊出血情况诊断牙周炎。共有829名研究对象在两到四年后重新接受第二次检查。
第一次的检查结果显示,13.7%的研究对象在“健康/牙龈炎”行列,38.7%的研究对象患有“轻度”牙周炎,18.3%的研究对象患有“中度”牙周炎,18.3%的研究对象患有“重度”牙周炎,10.9%的研究对象为无牙颌。对于未读过大学及不锻炼身体的男性,患牙周炎的可能性明显增加。平均而言,牙周病较重者为年老者以及较胖者,他们大多数为吸烟者,非白种人,而且基本不用牙线,不看牙医。健康牙龈或者牙龈炎的男性 25(OH)D的平均水平为23.5ng/ml,PTH总水平为 28.2 pg/ml,牙周炎较重的分别为22.4 ng/ml 和32.5 pg/ml,牙齿缺失的分别为 21.2 ng/ml 和34.4 pg/ml。首次拜访牙医时,那些患有较重牙周炎的男性,其25(OH)D和PTH的水平较低,但是它们与牙周炎的进展无关,另一方面,横断面上骨代谢标志物与牙周炎的严重程度无关,但是与那些牙周炎并未减轻甚至还在发展的男性患者相比,男性牙周炎减轻时,其骨代谢标志物的水平变得较低。
Dr. Schulze-Spate指出,该研究设计缺乏参与者在第一次拜访牙医之后是否接受了牙周治疗的信息。总体而言,该研究只显示二者之间存在关联,仍需更多地研究进一步扩展我们的发现。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













好文章,还会关注
82
#JCE#
70
#骨代谢标志物#
74
#代谢标志物#
105
#标志物#
58
#JCEM#
57
看看
146
#骨代谢#
0
#牙周#
44