Adv Mater:理化所亲疏水复合敷料用于促进伤口愈合研究获进展
2018-12-27 佚名 中国科学院理化技术研究所
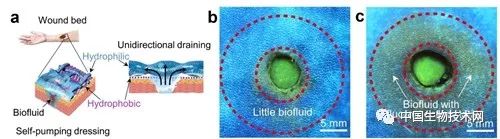
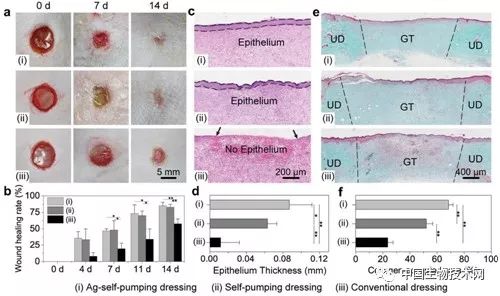
<div>伤口敷料在伤口周围微环境的生物流体<a class="channel_keylink" href="//www.sandwebs.com/guideline/list.do?q=%E7%AE%A1%E7%90%86" target="_blank">管理</a>中起着至关重要的作用,会直接影响伤口愈合的快慢。传统的伤口敷料材料如棉质纱布、聚合物纤维、多孔海绵等通过吸收来进行伤口生物流体的<a class="channel_keylink" href="//www.sandwebs.com/guideline/list.do?q=%E7%AE%A1%E7%90%86" target="_blank">管理</a>,由于这些材料本征的亲水性,生物流体会残留在伤口与敷料之间,进而泡软新生组织与伤周组织,降低组织强度,增加<a class="channel_keylink" href="//www.sandwebs.com/guideline/list.do?q=%E6%84%9F%E6%9F%93" target="_blank">感染</a>风险,阻碍伤口愈合。为此,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#敷料#
64
#研究获进展#
55
#伤口愈合#
62