Plos One:人类神经干细胞系源的外泌体miRNA内容物,化学计量法和转移的研究
2016-02-17 exsome exsome
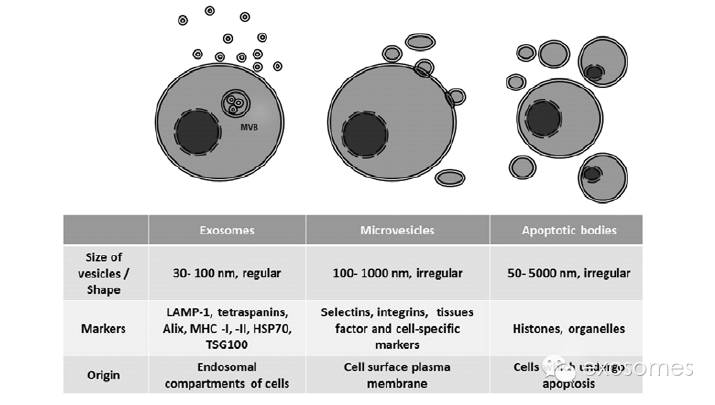
外泌体是由多种细胞类型分泌的小胞膜囊泡(30-100nm),并且直到最近才作为细胞间沟通的新途径出现,它们是 RNA和蛋白质的天然运载体,使得它们作为一种有吸引力的潜在治疗性运载工具 miRNA是短链非编码 RNA ,可调节生物学过程,并且被发现存在于外泌体中,这里我们描述了来源于人类神经干细胞( hNSCs )的外泌体中的 miRNA ,我们选择的 hNSCs 系是克隆的,有条件限制的,永
外泌体是由多种细胞类型分泌的小胞膜囊泡(30-100nm),并且直到最近才作为细胞间沟通的新途径出现,它们是 RNA和蛋白质的天然运载体,使得它们作为一种有吸引力的潜在治疗性运载工具
miRNA是短链非编码 RNA ,可调节生物学过程,并且被发现存在于外泌体中,这里我们描述了来源于人类神经干细胞( hNSCs )的外泌体中的 miRNA ,我们选择的 hNSCs 系是克隆的,有条件限制的,永生化的细胞系,符合良好的操作规范( GMP ),以及英国脑卒中和严重肢体缺血病人的临床试验,通过使用下一代测序( NGS )技术我们发现外泌体和细胞制剂中多种 miRNA 的存在,很多 miRNA 在外泌体中富集,表明细胞特异性将其释放于细胞外,尽管外泌体被证明含有 miRNA ,但每一种特定的 miRNA 在外泌体中的拷贝数的定量仍不清楚
我们通过实时定量PCR 来定量高度穿梭的外泌体中的 miRNA 亚型( hsa-mir-1246 )来评估在每份外泌体中的化学计量,此外,我们通过 3 ’ 非编码区双荧光素酶报告基因试验测量荧光素酶表达的减少来确认它的功能转移,总之,NGS 分析可用来识别一组特殊的 hNSCs 来源的外泌体 miRNA ;含量最丰富的可识别的 miRNA 中的一种, hsa-miR-1246 ,可对其进行化学计量和功能转移分析来支持外泌体 miRNA 传递的生物学相关性
miRNA在功能上抑制靶基因 mRNA 通过结合到它们的 3 ’ 非编码区(3 ’ UTR),一种单一的 miRNA 可能靶向作用于数百种 mRNA ,它通过外泌体转移可以绕过受体细胞的转录调控,并提供一种相对直接的调控方式。外泌体 miRNA 拷贝数的化学计量分析可能有助于深入了解基于 miRNA 的细胞间通讯的意义
由于外泌体是亚衍射极限粒子,他们的定量是具有挑战性的,因此不能通过光学显微镜或流式细胞术来直接计量,最近,纳米粒子跟踪分析(NTA )已被用来作为一种定量分析的新型系统,可分析大小在 30-1000nm 的粒子以及追踪他们的布朗运动来估计大小分布
技术的快速进步使得全面高效研究miRNA 的表达成为可能,其中下一代测序技术( NGS )可同时发现新的 miRNA 以及确定已知 miRNA 结合样本间的不同表达的评估;一旦候选miRNA/靶基因对被识别,他们的功能分析可以通过用miRNA模拟试验验证,miRNA/靶基因3’UTR介导的下调可用一种双荧光素酶报告基因在体外进行测量
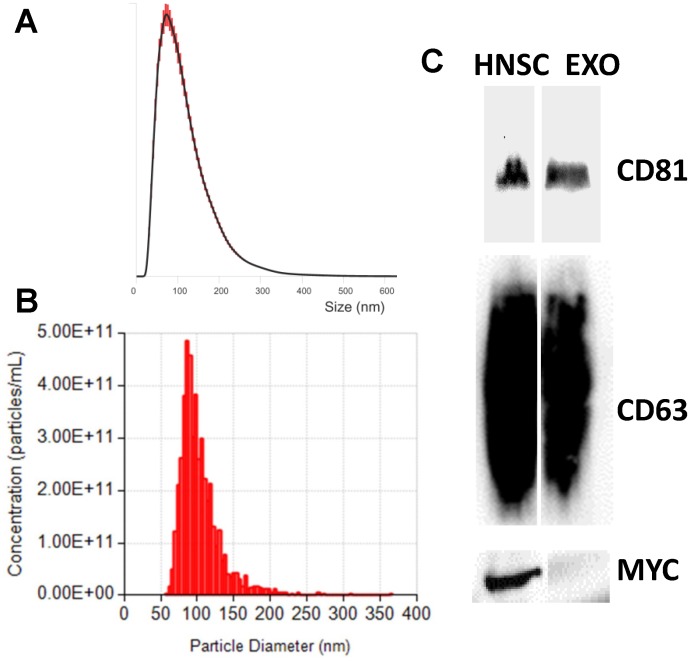
(1 ) Fig 1.The characterization of exosomes derived from hNSCs
首先我们从hNSC 系 CTX0E03 的培养基中提取外泌体,外泌体的大小分布和数量分析使用 NTA ( Fig1A )和qNano ( Fig1B )两种技术方法,我们的制备物有一个模式大小,95nm ±2.3SEM(NTA)和86nm±2.2SEM( qNano ) ;为了确证我们分离到外泌体,进行了WB 试验 ( Fig1C), 外泌体标志物为CD63,CD81 ,细胞标志物为 MYC
Size distribution of exosomes analyzed with the NTA (A) and qNano (B), representative traces. In agreement with exosome sizes, isolated exosomes had a mode of approximately 100 nm. (C) Molecular characterization of exosomes and producer hNSCs by Western blotting. Protein extracts from hNSCs and exosomes were assessed using antibodies against exosomal protein markers (CD81 and CD61), and hNSC protein marker (MYC).
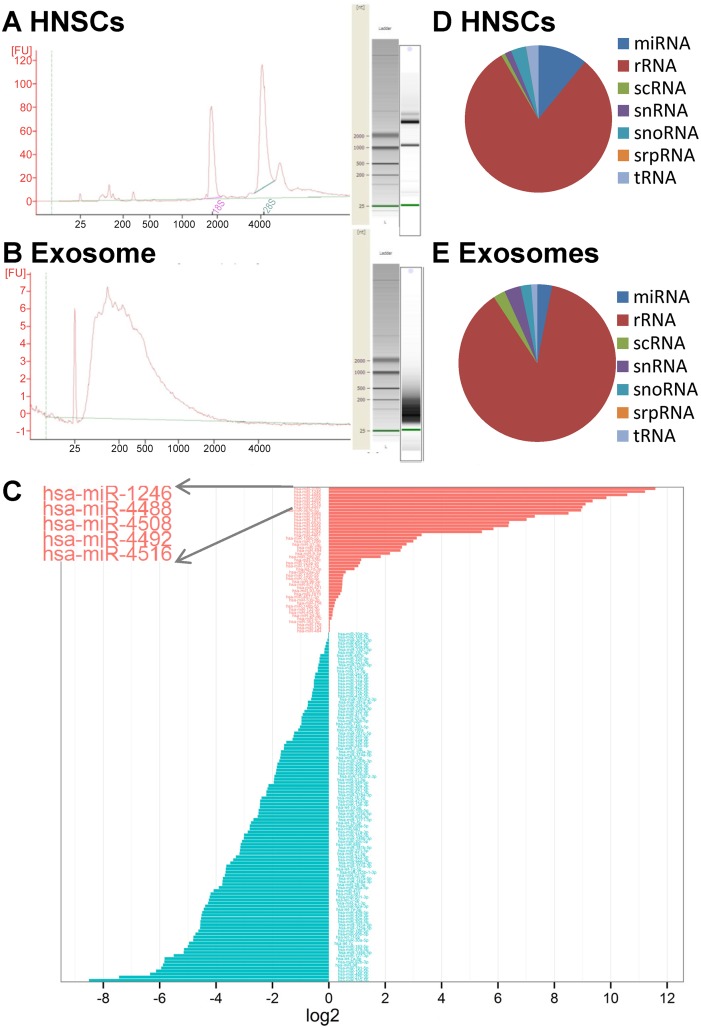
( 2 ) Fig 2. MiRNA next generation sequencing
细胞的( Fig.2A )和外泌体的( Fig.2B )的总 RNA用 Agilent2100 生物分析仪处理,对应的虚拟凝胶图像由软件生成来描述电泳图谱
(Fig.2C ) 描述了相对于hNSC 而言,外泌体中有差异的 miRNA 的分布,在外泌体中优先释放的即丰度最高的 5 种为 miRNA 为Hsa-miR-1246, hsa-miR-4488,hsa-miR-4508, hsa-miR-4492 and hsa-miR-4516 ,根据此发现和之前的报道,说明 miRNA 传送到外泌体似乎不是一个随机的过程; ( Fig.2 D和 2E) 已获取的读序被绘制来确定分别源于不同类别RNA 例如 rRNA, tRNA, snRNA 和 snoRNA 的分布 ,总体来说,一个重要部分是来自 rRNA 和 tRNA ;
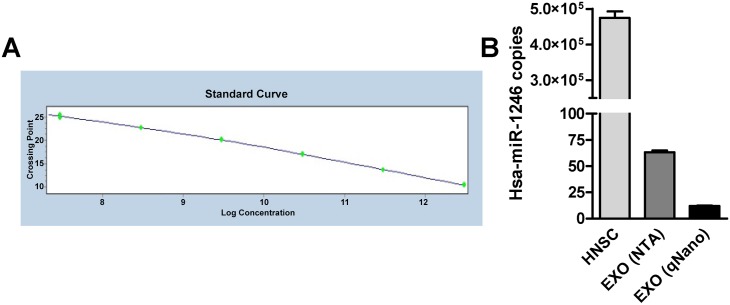
(3) Fig 3. Absolute quantification of selected miRNA
(Fig.3A ) 研究的 miRNA 的已知浓度通过核酸260nm 波长的分光光度法测量,用它的分子量转换为拷贝数,制作成一个标准曲线,任何测试样品中研究的 miRNA 的绝对浓度通过标准曲线中的PCR 信号(交叉点, Cp )的简单插值来确定;最丰富的 miRNA 中的一种, hsa-miR-1246 被选择,在每份外泌体中它的拷贝数用 qRT-PCR测量;
(Fig.3 B ) 显示了每份hNSC 和每份外泌体的 hsa-miR-1246 拷贝数的数量,外泌体粒子定量用两种独立的方法, NTA和 qNano ,细胞数目定量用血球计数器;总体上,在每份外泌体中被选择的 miRNA 至少有10 个拷贝数,对比于每份 hNSC 中 4.75×10 5 ± 18×10 3 SEM 的拷贝数
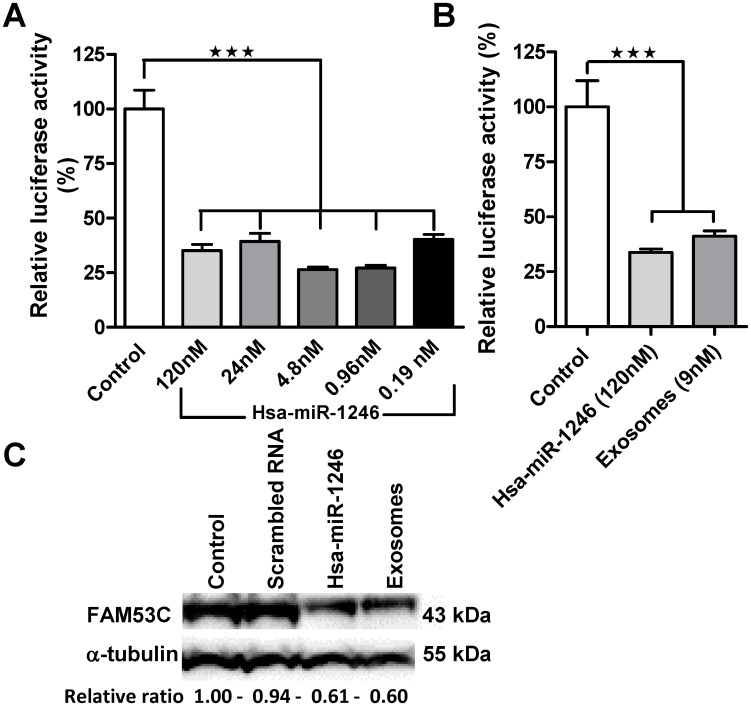
(3) Fig 4. Functional transfer assessment of exosomal miRNA
( Fig 4 A) 研究者为了验证 hNSC外泌体制备物可以转移一定的 miRNA 在一个功能性的水平,足以介导生物效应,开发了一种体外方法,具体是由3 ’ UTRFAM53C(通过大量预测算法确定为 hsa-miR-1246 的 top ranking靶 mRNA )接触hNSC 外泌体制剂和 hsa-miR-1246 mimic 后引起荧光素酶蛋白表达的减少,用 Hela细胞的 hsa-miR-1246 / FAM53C在体外的报告荧光素酶检测方法测量表达的减少,观察到相对荧光素酶活性从 73.59% ± 1.15 SEM 减少到 59.77% ± 2.32 SEM ;
( Fig 4 B) Hela细胞 用外泌体制备物预处理,随后用 FAM53C3 ’ UTR双荧光素酶质粒转染,对照孔用 FAM53C3 ’ UTR双荧光素酶质粒转染,或为阳性 miRNA 或为阴性 miRNA ,探测到相对荧光素酶活性中一个 58.79% ± 2.39 SEM 显著性的减少
( Fig 4 C )进行了 FAM53C 的 WB分析,这种蛋白质在未经 miRNA 处理的 Hela细胞 和 hsa-miR-1246 mimic 以及经外泌体处理的 Hela细胞 中差异表达
总结:研究外泌体 miRNA 亚型的识别,选定的外泌体 miRNA 的化学计量以及它的转移,可以在分子机制,来源于hNSC 的外泌体 miRNA 的生理相关性,作为治疗应用的适用性等方面提供很有价值的认识
原始出处:
Stevanato L, Thanabalasundaram L, Vysokov N, Sinden JD.Investigation of Content, Stoichiometry and Transfer of miRNA from Human Neural Stem Cell LineDerived Exosomes. PLoS One. 2016 Jan 11;11(1):e0146353
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#干细胞系#
64
#miR#
67
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
95
非常好,希望能详细些
101
#Plos one#
56
#miRNA#
62
#细胞系#
61
#神经干细胞#
48