Genome Bio:解肿瘤复发之惑,测突变功不可没!
2015-03-26 Zhang JL译 MedSci原创
来自新加坡的多学科医生和科学家团队发现了结直肠癌扩散到肝脏的特征性基因变化。这一发现意义重大,有助于基于肿瘤的基因变化为每一位结直肠癌患者开发个性化诊断方法。 该研究小组成员包括新加坡国立癌症中心 (NCCS)、新加坡综合医院(SGH)、Duke-NUS研究生医学院(Duke-NUS)、新加坡A * STAR基因组研究所(GIS)和新加坡国立大学(NUS)的癌症科学研究所。该项研究结果在线发表在最
来自新加坡的多学科医生和科学家团队发现了结直肠癌扩散到肝脏的特征性基因变化。这一发现意义重大,有助于基于肿瘤的基因变化为每一位结直肠癌患者开发个性化诊断方法。 该研究小组成员包括新加坡国立癌症中心 (NCCS)、新加坡综合医院(SGH)、Duke-NUS研究生医学院(Duke-NUS)、新加坡A * STAR基因组研究所(GIS)和新加坡国立大学(NUS)的癌症科学研究所。该项研究结果在线发表在最新一期Genome Biology杂志上。
结直肠癌是新加坡最常见的癌症,而且其发病率呈现逐渐上升的趋势。大多数病人在最初诊断的时候还是疾病早期阶段。然而,这些病人中有一定比例的人在接受结肠手术后一至三年内发生肿瘤复发或转移,而转移最常见发生在肝脏。如果及早发现,通过手术切除肝转移造并且获得治愈的可能性仍然是存在的。
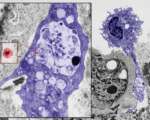
这一个新加坡团队应用领先的DNA测序工具,对大肠癌肝脏转移的相关特征性基因改变进行检测。所用的检测方法中部分是他们自主开发的,包括由Duke-NUS和GIS研发的专门实验室技术和计算方法。
在纳入统计的750个基因中,研究人员发现每一个人的癌症有一组独特的包括15个关键基因的突变。虽然这些特异性突变在两个不同的病人中几乎没有重叠,但大多数结肠肿瘤患者的这些突变与其肝转移转移灶中的突变是一致的。研究人员试图利用这种生物现象基于基因信息开发新的诊断测试方法,以第一时间在切除的肿瘤中搜索和识别癌症的早期转移的可能。
“癌症幸存者都恐惧自己的癌症复发。即使这一切真的发生,我们仍然有机会通过早期诊断来治愈这些结肠癌患者。该研究成果能够对病人的生活质量产生重大影响,并提供他们所接受治疗的精度,”该研究的作者、SGH结直肠外科带头人Tang Choong Leong教授说。
该研究的作者、NCCS 医学肿瘤学家以及GIS临床科学家Iain Tan博士解释说:“基于这项研究结果,我们为每一位结直肠癌患者定制个人诊断测试。我们将利用存在于每一个患者中独特的基因变异,就像条形码或拇指指纹一样,我们开发创新的诊断方法以监测和早期诊断癌症复发。”该研究团队被授予国家医学研究理事会(NMRC)的资助以进一步研发这一诊断测试。虽然Tan博士对这一项研究结果持乐观态度,但他强调必须意识到这种研发工作依然需要数年时间才能取得更大的进展。
原始出处:
Iain Beehuat Tan, Simeen Malik, Kalpana Ramnarayanan, John R McPherson, Dan Liang Ho, Yuka Suzuki, Sarah Boonhsui Ng, Su Yan, Kiat Hon Lim, Dennis Koh, Chew Min Hoe, Chung Yip Chan, Rachel Ten, Brian KP Goh, Alexander YF Chung, Joanna Tan, Cheryl Xueli Chan, Su Ting Tay, Lezhava Alexander, Niranjan Nagarajan, Axel M Hillmer, Choon Leong Tang, Clarinda Chua, Bin Tean Teh, Steve Rozen, Patrick Tan. High-depth sequencing of over 750 genes supports linear progression of primary tumors and metastases in most patients with liver-limited metastatic colorectal cancer. Genome Biology, 2015; 16 (1) DOI:10.1186/s13059-015-0589-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肿瘤复发#
62
#Bio#
53
期待有更多研究
172
不错,学习了
124
应该好好学习
150
值得学习
158
好文字
140
是对原发灶和转移灶相关的克隆进化选择学说的一个补充。
117