Ann Oncol:MEK抑制剂trametinib对KRAS突变的非小细胞肺癌的II期临床研究
2015-03-03 范伟译 MedSci原创
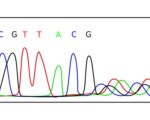
背景:KRAS突变在25%的非小细胞肺癌(NSCLC)患者上检测到,对这一亚群的靶向治疗药物还没有得到批准的。Trametinib,选择性变构的MEK1/MEK2抑制剂,在KRAS突变的非小细胞肺癌的临床前和临床研究上具有活性。我们报告了一项trametinib相比于多西他赛用于KRAS突变的晚期非小细胞肺癌患者的II期临床研究。 患者和方法:符合条件的患者为组织学证实为KRAS突变的非小细胞肺
背景:KRAS突变在25%的非小细胞肺癌(NSCLC)患者上检测到,对这一亚群的靶向治疗药物还没有得到批准的。Trametinib,选择性变构的MEK1/MEK2抑制剂,在KRAS突变的非小细胞肺癌的临床前和临床研究上具有活性。我们报告了一项trametinib相比于多西他赛用于KRAS突变的晚期非小细胞肺癌患者的II期临床研究。
患者和方法:符合条件的患者为组织学证实为KRAS突变的非小细胞肺癌患者先前采用铂类为基础的化疗治疗的,患者随机按2:1分配为trametinib(2 mg,每日一次口服)或多西他赛(75 mg/m2 静脉注射,每3周一次)。主要终点是无进展生存期(PFS)。这项研究因92例无进展生存期事件过早终止,该事件表明针对于无进展生存期trametinib相比于多西他赛超过了无效的边缘。
结果:129例KRAS突变的非小细胞肺癌患者随机分配;86例接受trametinib ,43例接受多西他赛。在trametinib组,无进展生存期中位数为12周,在多西他赛组,无进展生存期中位数为11周(风险比[HR] 1.14;95% CI 0.75-1.75;P = 0.5197)。因为数据的不成熟,总生存期的中位数,在trametinib组为8个月,不及多西他赛组(HR 0.97;95% CI 0.52-1.83;P = 0.934)。trametinib组有10(12%)例部分响应(PR),多西他赛组有5(12%)例部分响应(P = 1.0000)。大于或者等于20%的trametinib治疗的患者最常见的不良反应(AE)为皮疹,腹泻,恶心,呕吐,疲劳。trametinib组最常见的3级治疗相关的不良反应为高血压,皮疹,腹泻,乏力。
结论:针对于先前得到治疗的KRAS阳性突变的非小细胞肺癌患者,trametinib与多西他赛相比显示了相似的无进展生存期和响应速率。
原始出处
Blumenschein G Jr1, Smit EF2, Planchard D3, Kim DW4, Cadranel J5, De Pas T6, Dunphy F7, Udud K8, Ahn MJ9, Hanna NH10, Kim JH11, Mazieres J12, Kim SW13, Baas P14, Rappold E15, Redhu S15, Puski A16, Wu FS15, Jänne PA17.A randomized phase 2 study of the MEK1/MEK2 inhibitor trametinib (GSK1120212) compared with docetaxel in KRAS-mutant advanced non-small cell lung cancer (NSCLC).Ann Oncol. 2015 Feb 26. pii: mdv072.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
54
#非小细胞#
59
#Trametinib#
72
#MET#
73
#II期临床研究#
63
#MEK#
64
#I期临床#
54
#抑制剂#
55
很不错学习了
76
#TRA#
78