NEJM:Morgagni疝致肺塌陷-案例报道
2016-05-12 Mechront 译 MedSci原创
患者男,54岁,既往有大脑性麻痹和精神损伤,以急性呼吸窘迫为主要表现,此外还有干咳,不伴发热。查体:辅助肌参与呼吸,右胸部扩张度下降,右胸部未闻及呼吸音,但可以听到肠鸣音。患者轻度缺氧。胸片:右胸部基本上完全浑浊不透明,可见充气肠袢,延伸至主动脉弓水平。3个月前的影像学检查提示:小的右侧膈疝。此次行胸部CT检查:证实了右侧横膈疝的存在,缺陷隔膜直径约为4.5厘米。右侧胸腔内可见大量腹部肠内容物,包
患者男,54岁,既往有大脑性麻痹和精神损伤,以急性呼吸窘迫为主要表现,此外还有干咳,不伴发热。
查体:辅助肌参与呼吸,右胸部扩张度下降,右胸部未闻及呼吸音,但可以听到肠鸣音。
患者轻度缺氧。
胸片:右胸部基本上完全浑浊不透明,可见充气肠袢,延伸至主动脉弓水平。
3个月前的影像学检查提示:小的右侧膈疝。
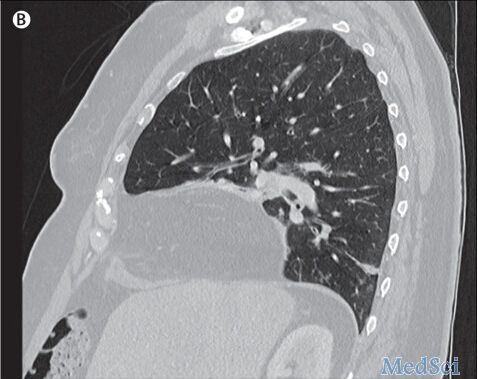
此次行胸部CT检查:证实了右侧横膈疝的存在,缺陷隔膜直径约为4.5厘米。
右侧胸腔内可见大量腹部肠内容物,包括右半结肠、阑尾、小肠、肠系膜脂肪和大网膜。右肺完全倒塌,粘液堵塞右主支气管。纵隔轻微向左移位,与重度肺塌陷伴疝的表现一致,可能与近端支气管的阻塞有关。
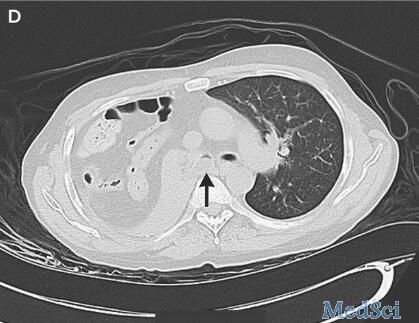

考虑到膈疝的位置,Morgagni疝(先天性胸骨旁疝)的可能性较大,这种疝通常是先天性的,随着时间可以变大,就如本案例一样。
与患者和家属沟通后,尊重他们的意愿,没有进行外科修复。
原始出处:
Muhammad Yasin, M.D., and James C. Reed, M.D.Diaphragmatic Hernia Causing Lung Collapse.N Engl J Med 2016; 374:1874May 12, 2016DOI: 10.1056/NEJMicm1415660
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







不错哦继续关注
0
继续学习
60
继续关注
68
深入学习,好文值得点赞!
59
#疝#
56