Gastroenterology:结直肠癌的分子分型可预测患者生存期
2013-09-10 佚名 丁香园
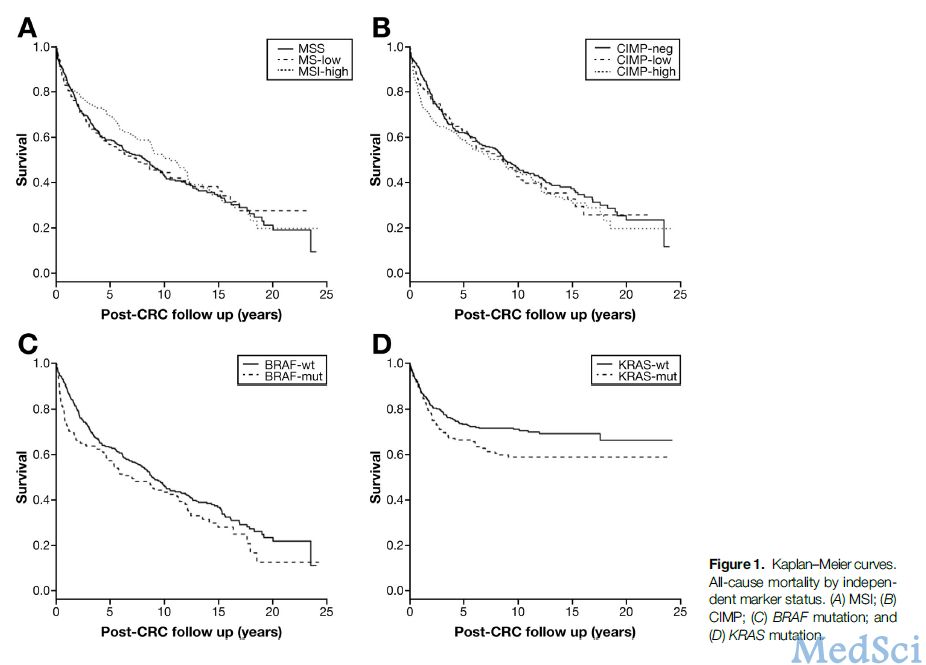
结直肠癌是一个异质性分型的集合体。其发病是一系列不同遗传事件和表观遗传学事件不同组合所造成的结果。越来越多的证据支持根据个体存在微卫星不稳定性的情况、CpG岛甲基化表型、体细胞BRAF突变情况及体细胞KRAS突变情况将结直肠癌分为不同的分子亚型。 例如与微卫星灶稳定或微卫星灶不稳定性程度低的结直肠癌患者相比较,微卫星不稳定性程度高的患者结直肠癌更多定位于近端结肠、临床分期较低级、分化程度较高且肿
结直肠癌是一个异质性分型的集合体。其发病是一系列不同遗传事件和表观遗传学事件不同组合所造成的结果。越来越多的证据支持根据个体存在微卫星不稳定性的情况、CpG岛甲基化表型、体细胞BRAF突变情况及体细胞KRAS突变情况将结直肠癌分为不同的分子亚型。
例如与微卫星灶稳定或微卫星灶不稳定性程度低的结直肠癌患者相比较,微卫星不稳定性程度高的患者结直肠癌更多定位于近端结肠、临床分期较低级、分化程度较高且肿瘤组织中淋巴细胞浸润较多。CpG岛甲基化程度高的结直肠癌多定位于近端结肠,患者年龄偏大,肿瘤分化程度低并通常伴有微卫星不稳定性程度高。
目前临床常用的根据肿瘤解剖情况进行分类的TNM分期无法很好的进行组织异质性的分类,从而无法对患者的预后及转归做出准确判断,这就使得结肠癌分子分型成为必要。
美国犹他州盐湖城犹他大学癌症研究所胃肠病学系N. JEWEL SAMADDER等人在前人的研究基础上利用大样本验证了结直肠癌患者的临床病理特征与结直肠癌分子分型之间的相关性,发现目前提出的分子分型可以发挥判断结直肠癌TNM分期及生存期的作用,但也指出为了验证上述结论仍需要进行更多的临床数据验证,这一结果发表在2013年7月的Gastroenterology上。
作者从已建档的732名结直肠肿瘤患者取样并评估其特征,如微卫星稳定、微卫星不稳定性程度的高低、CpG岛甲基化程度高或低、CpG岛甲基化表型阴性、BRAF和/或KRAS突变的阴性或阳性。从563(77%)肿瘤患者中收集到了信息标志物数据,分别归纳为下列整合成的途径。
经典型(微卫星稳定、CpG岛甲基化表型阴性、BRAF突变阴性以及KRAS突变阴性,n?170);替换型(微卫星稳定、CpG岛甲基化表型程度低、BRAF突变为阴性、KRAS突变阳性,n?58);锯齿型(任何程度的微卫星不稳定、CpG岛甲基化程度高、BRAF突变为阳性、KRAS突变阳性,n?142);未定义型(n?193)。多变量调整Cox比例风险回归模型用于评估指标间的相关性。
结果显示患者平均年龄(P?=0.03)、肿瘤的解剖结构(P?=0.0001)和分级(P?=0.0001)与整合路径分配密切相关。结直肠癌患者死亡率与经典路径、替换路径和锯齿型路径并无明显相关性,而与未定义路径下面的亚型(微卫星稳定或微卫星不稳定性程度低、CpG岛甲基化阴性、BRAF突变阴性、KRAS突变阳性)有关(n?=96例,与经典型路径相比较,相对风险系数?1.76,95%可信区间1.072-0.89)。
由此可见,结直肠癌患者的临床病理特征与分子分型之间的存在明显相关性。然而这些分子变化特征是否影响预后还需要进一步的实验研究。
原文阅读
Samadder NJ, Vierkant RA, Tillmans LS, Wang AH, Weisenberger DJ, Laird PW, Lynch CF, Anderson KE, French AJ, Haile RW, Potter JD, Slager SL, Smyrk TC, Thibodeau SN, Cerhan JR, Limburg PJ.Associations between colorectal cancer molecular markers and pathways with clinicopathologic features in older women.Gastroenterology. 2013 Aug;145(2):348-356.e2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Gastroenterol#
40
#患者生存#
54
#GAS#
42
#AST#
55
#生存期#
52
#结直肠#
49
#Gastroenterology#
48