JACR:哪些甲状腺结节应该穿刺?美国放射学会发布白皮书
2017-07-14 肿瘤资讯编辑部 肿瘤资讯
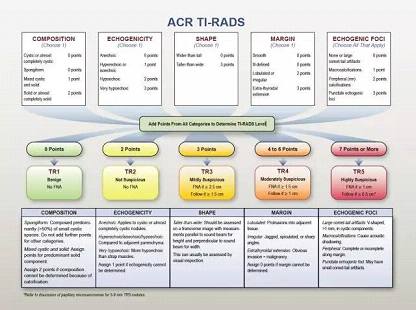
随着甲状腺超声检查的普及,甲状腺结节的检出率非常高,但大多数的结节都是良性的。尽管多数的甲状腺结节进行了穿刺活检,但真正是恶性或需要手术来明确诊断的结节很少。近期,美国放射学会(ACS)发布白皮书:ACS甲状腺影像报告和数据系统(Thyroid Imaging Reporting and Data System,TI-RADS),指导临床医生如何根据超声结果来进行甲状腺结节管理。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#穿刺#
61
#放射学#
62
#ACR#
58
#白皮书#
59
继续学习。
88
学习,谢谢分享
88
6
90