JACC:低血流状态是重度主窄患者TAVR术后死亡率的独立预测因子
2013-08-26 箫砚 dxy
表1,不同组别的30天死亡率 表2,不同组别的全因死亡率与心血管事件死亡率曲线 表3,不同组别的全因死亡率与心血管事件死亡率曲线 表4,LF-LG组别分为LF-LG-NEF与LF-LG-LEF亚组之后,不同组别全因死亡率与心血管事件死亡率曲线 表注:1,NF-HG:正常血流状态NF (SVi >35 ml/m2),高瓣膜压差HG (
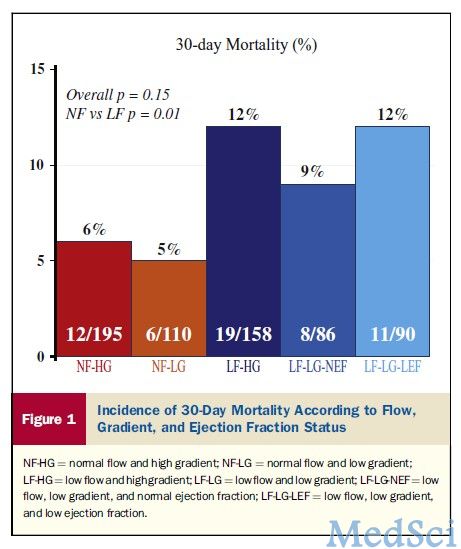
表1,不同组别的30天死亡率
表注:1,NF-HG:正常血流状态NF (SVi >35 ml/m2),高瓣膜压差HG (≥40 mm Hg) ; 2,NF-LG:正常血流状态NF与低瓣膜压差LG (<40 mm Hg); 3,LF-HG:低血流状态LF (SVi <35 ml/m2) 与高瓣膜压差HG ; 4,LF-LG:低血流状态LF 与低瓣膜压差LG (LF-LG);5,LF-LG-LEF:LF-LG 合并低 LVEF (<50%);6,LF-LG-NEF:LF-LG合并正常LVEF (≥50%)。
研究表明,心脏射血分数正常、低血流状态、瓣膜压差较低的患者手术治疗预后要好于药物治疗。但是,低血流状态、左室射血分数对经导管瓣膜置换术的影响尚不可知。此外,有研究表明,术前低瓣膜压差与经导管主动脉瓣膜置换术之间增高的死亡率有关。【原文下载】
本研究旨在分析经导管主动脉瓣膜置换术前血流状态、左室射血分数以及瓣膜压差对于患者死亡率的影响。研究人员分析了639名患者的临床以及超声心动图数据,这些患者曾因重度主动脉瓣狭窄接受经导管瓣膜置换术。研究的主要终点为全因死亡率,次要终点是心血管事件死亡率与30天死亡率。
研究结果显示,低血流状态(左室射血分数以及瓣膜压差不低)是重度主动脉狭窄患者行经导管主动脉瓣膜置换术后早期与晚期死亡率的独立预测因子。患者的危险分层应纳入每搏输出量。
原始出处:
Le Ven F, Freeman M, Webb J, Clavel MA, Wheeler M, Dumont E, Thompson C, De Larochellière R, Moss R, Doyle D, Ribeiro HB, Urena M, Nombela-Franco L, Rodés-Cabau J, Pibarot P.Impact of low flow on the outcome of high-risk patients undergoing transcatheter aortic valve replacement.J Am Coll Cardiol. 2013 Aug 27;62(9):782-8. doi: 10.1016/j.jacc.2013.05.044. Epub 2013 Jun 12. 【原文下载】
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AVR#
56
#JACC#
50
#预测因子#
42
#ACC#
40
#术后死亡率#
68