Lancet:呼吸急促、喉咙痛一周病例报道(Morgagni疝)
2016-01-31 Mechront 译 MedSci原创
患者女,56岁,因“呼吸急促、喉咙痛一周”就诊。既往史:肥胖、2型糖尿病、高血压。个人史:吸烟。查体:无发热;心音减弱;双侧肺基底闻及哮鸣音和羊音。辅助检查:呼吸室内空气的情况下血氧饱和度81%,最低达71%。白细胞计数在正常范围内。胸片示右侧心膈角大块模糊影(图A)。考虑诊断肺炎,并进行相关肺炎治疗。但是CT示:嵌顿性Morgagni疝;右前隔膜缺损,最宽处22.6cm,大网膜突入胸腔;没有肺炎
患者女,56岁,因“呼吸急促、喉咙痛一周”就诊。
既往史:肥胖、2型糖尿病、高血压。
个人史:吸烟。
查体:无发热;心音减弱;双侧肺基底闻及哮鸣音和羊音。
辅助检查:呼吸室内空气的情况下血氧饱和度81%,最低达71%。白细胞计数在正常范围内。胸片示右侧心膈角大块模糊影(图A)。
考虑诊断肺炎,并进行相关肺炎治疗。
但是CT示:嵌顿性Morgagni疝;右前隔膜缺损,最宽处22.6cm,大网膜突入胸腔;没有肺炎迹象(图B)。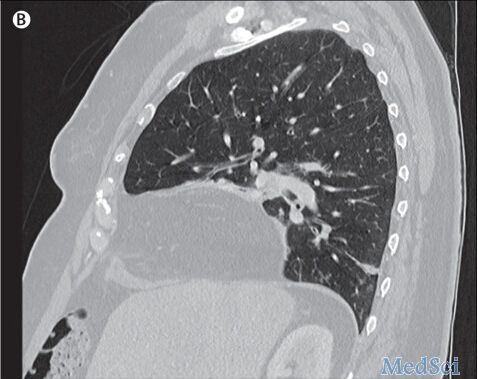
Morgagni疝又称先天性胸骨旁疝,多为成年女性、肥胖者,右侧多见,疝入的器官以大网膜多见,有时为结肠。
结合该患者实际情况,医生认为微创修复会比传统的开放性手术更具优势。于是患者开始家庭氧疗,并在医院进行了经腹腔镜疝修补术,使用符合材料修补了缺损的膈肌。四周后患者不再进行家庭氧疗。
本例患者可能是巨大疝和吸烟史的基础上并发病毒性呼吸道感染,导致低氧血症。
Morgagni疝是由于构成膈肌的肋骨部分的两束肌肉的先天性缺陷造成的,疝囊常见于右边,可以包含小肠、横结肠、大网膜,胃和肝少见。无症状的Morgagni疝患者通常是偶然发现该疾病;不过当症状出现时,患者常会有反复的呼吸道感染和不同程度的呼吸衰竭。
若患者出现长时间的呼吸急促,胸片提示右心膈角病变,医生应考虑膈疝的可能。对没有症状偶然发现的患者,也应该行修复术,以减少呼吸困难和窒息风险。
原始出处:
Morgagni's hernia in a hypoxaemic adult.Adam G R Humble,Dr Cliff B Sample.The Lancet.Available online 29 January 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Lancet#
56
#喉咙痛#
68
#呼吸急促#
61
赞
128
#疝#
58
赞
124
可以学习下
80