NEJM:转移性黑色素瘤治疗后的一个罕见现象
2012-03-10 MedSci MedSci原创
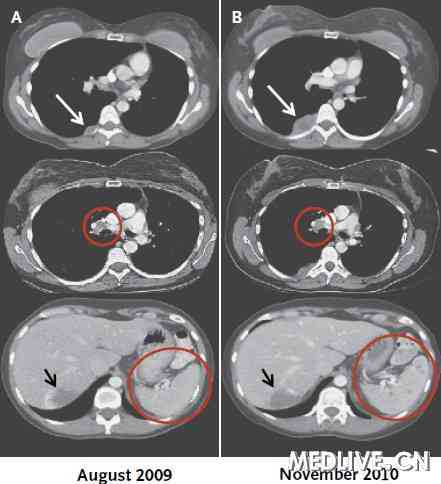
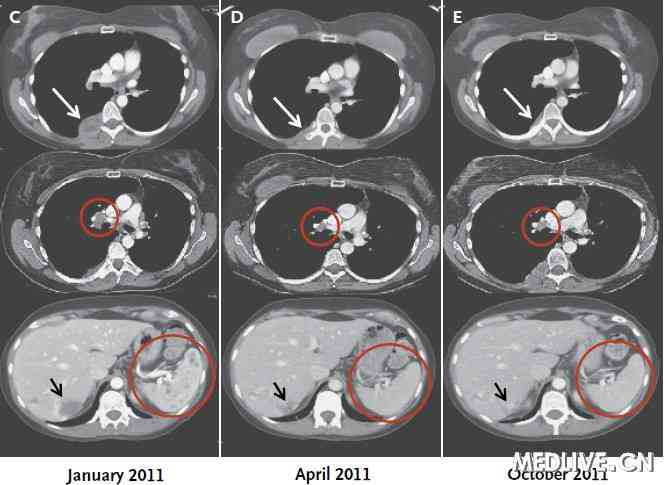
在癌症治疗后发生了一个罕见现象,病人局部放疗后出现系统性反应,这种情况被称为远端效应(abscopal effect),发生在一个患转移性黑色素瘤的40岁妇女身上,该妇女接受Ipilimumab(Yervoy,施贵宝)的免疫治疗。本文发表在3月8日的新英格兰杂志上。 病人是一位一直在工作的单身母亲,在放疗期间一直使用Ipilimumab进行维持治疗,治疗医生为纪念斯隆 - 凯特
在癌症治疗后发生了一个罕见现象,病人局部放疗后出现系统性反应,这种情况被称为远端效应(abscopal effect),发生在一个患转移性黑色素瘤的40岁妇女身上,该妇女接受Ipilimumab(Yervoy,施贵宝)的免疫治疗。本文发表在3月8日的新英格兰杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#色素#
41
#转移性黑色素瘤#
64
#转移性#
57
#罕见#
58
#黑色素#
45
#黑色素#
46