Cell Report:阻断氧气传感分子PHD2可抑制乳腺癌的转移
2015-07-31 sunshine 译 MedSci原创
比利时鲁汶大学研究人员发现,降低氧气传感分子PHD2的表达可削弱乳腺癌转移(扩散)到身体其他部位的能力。乳腺癌是女性癌症死亡的第二大死因,主要死于癌细胞的转移。这些表明,抑制PHD2可能在治疗乳腺癌方面具有潜在的价值。该研究成果发表于 Cell Reports。本研究首次检测了自发性乳腺癌模型(相比于以往的移植性肿瘤与人类癌症更相似)中阻断PHD2表达的作用。该研究还发现了基质成纤维细胞(支持并
比利时鲁汶大学研究人员发现,降低氧气传感分子PHD2的表达可削弱乳腺癌转移(扩散)到身体其他部位的能力。乳腺癌是女性癌症死亡的第二大死因,主要死于癌细胞的转移。这些表明,抑制PHD2可能在治疗乳腺癌方面具有潜在的价值。该研究成果发表于 Cell Reports。
本研究首次检测了自发性乳腺癌模型(相比于以往的移植性肿瘤与人类癌症更相似)中阻断PHD2表达的作用。该研究还发现了基质成纤维细胞(支持并促进癌细胞扩散的细胞)意想不到的作用。
Peter Carmeliet研究团队发现,PHD2的基因阻断可大幅减少乳腺癌的转移。尽管改善了乳腺癌的治疗方法,但是开发有效的治疗方法以阻断乳腺癌的转移仍是个巨大的挑战。他们的研究还表明,与以往并不理想的肿瘤模型实验结果相反,阻断PHD2的表达并不会促进肿瘤的生长,因此采用此方法治疗是安全的。
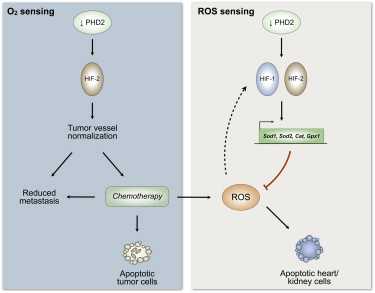
研究表明,抑制PHD2减少癌细胞扩散的两种机制:通过规范化肿瘤血管和抑制“肿瘤激活成纤维细胞”的激活。肿瘤中,PHD2支持成纤维细胞变得异常活跃,位于结缔组织之下,作为癌细胞的“高速公路”允许癌细胞扩散至远隔器官。然而,大多数的抗癌疗法都是针对癌细胞而非其相邻细胞——肿瘤激活成纤维细胞。事实上,并没有单一的治疗方法抑制这些成纤维细胞的活性以抑制癌细胞的转移。
Peter Carmeliet说道:“我们发现阻断PHD2 氧传感器以减少癌细胞转移的方式有两种:一是,阻断后有助于肿瘤中的血管恢复正常状态以减小癌细胞穿越血管壁的机会。二是,阻断后可切断“高速公路”防止癌细胞借助邻近激活成纤维细胞扩散。”
原始出处:
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
52
#阻断#
56
#Cell#
56
#PhD#
99
#PHD2#
52
PHD与肿瘤缺氧微环境是相关的
129