10种心电图,1句话牢记!
2015-08-24 日志 人人网
正常心电图: 1.没刻度的: 2. 有刻度的(临床常用): 纵向每一小格代表0.1mV,横向每一小格代表0.04s。(因为心电图机的灵敏度和走纸速度分别是1mV/cm和25mm/s.) P波:<0.25mV, <0.12s QRS波:0.06~0.10s PR间期:0.12~0.20s QT间期:<0.40s. HR(心率):60~100次/min.
正常心电图:
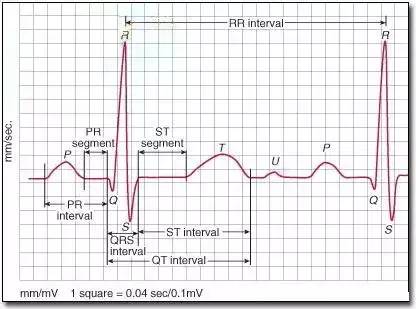
1.没刻度的:

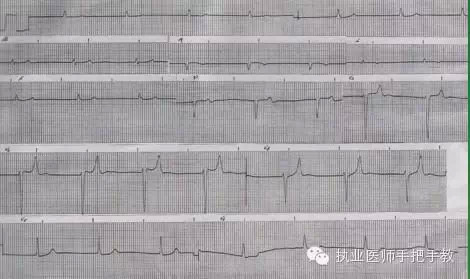
2. 有刻度的(临床常用):
纵向每一小格代表0.1mV,横向每一小格代表0.04s。(因为心电图机的灵敏度和走纸速度分别是1mV/cm和25mm/s.)
P波:<0.25mV, <0.12s
QRS波:0.06~0.10s
PR间期:0.12~0.20s
QT间期:<0.40s.
HR(心率):60~100次/min.
3.所有的12个导联(肢体导联Ⅰ,Ⅱ,Ⅲ,aVR,aVL,aVF;胸导联V1,V2,V3,V4,V5,V6):

各段意义:
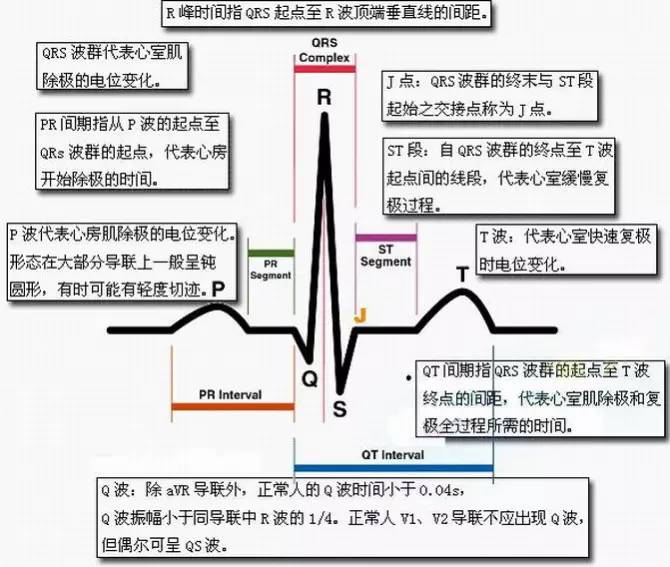
纵向每一小格代表0.1mV,横向每一小格代表0.04s。(因为心电图机的灵敏度和走纸速度分别是1mV/cm和25mm/s.)
10种心电图一句话牢记:
1,正常心电图:不用说了,它有可能是把那几个波和导联都斩一段下来,每一个波给你3个周期,分成几行给你看,要注意。(P,QRS,T波;PR,QT间期)
2,左心室肥大:只要看V5大于5格,是上下纵的5格(即V5导联QRS波>0.25mV)
3,右心室肥大:只要看V1大于2,格,是上下纵的2格(即V1导联QRS波中R/S>1,也就是R波>S波的幅度)
4,心房颤动:所有的P--P,Q--Q,R--R,S--S,T--T都没规律,也就是P波的位置上乱七八糟的。可发展为心室颤动。(即P波的位置被 大小不一的小f波取代,而QRS波正常)
心室颤动 :所有的P--P,Q--Q,R--R,S--S,T--T都没规律,正常QRS波消失,只剩下大小不一的小波。此时病人极度危险,随时心室骤停,应及时电除颤。
5,窦性心动过缓:P波正常,且每个心动周期,即两个P波之间,也叫P-P间期,都大于5个大格(25个小格),是左右横的格。
(即P-P间期>1.00s,可算出心率<60次/min )
6,窦性心动过速:P波正常,且每个心动周期都小于3个大格(15个小格),是左右的格。(即P-P间期<0.60s,可算出心率>100次/min )
7,房性期前收缩:前面几个正常的波,接着一个波提前(注意:这个波的pqrst形状是正常的,只是提前罢了),接下去又是正常的波。
8,室性期前收缩:前面几个正常的波,接着一个波提前(注意:这时候R波变宽),接下去又是正常的波。
9,典型心肌缺血:V4,V5,V6的ST段下移。
10,急性心肌梗死:Q波增宽+ST段弓背向上抬高,注意:前壁看V1,V2,V3,V4,V5,V6;下壁看Ⅱ,Ⅲ,aVF。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










简单,易懂,好东西。
123
心肌缺血不像以前见到的
206
好东西
48
实用
164
??
143