J Infect Dis:张云研究组揭示细胞清除病原体新策略和效应分子
2017-04-29 佚名 昆明动物研究所
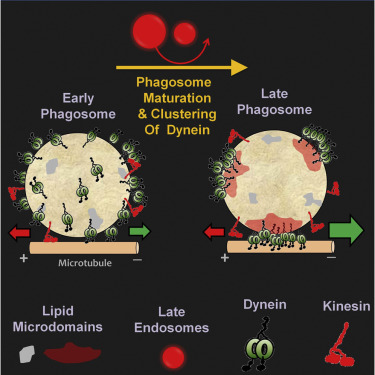
胞内细菌,病毒等细胞内感染病原体能够利用多种策略适应以及改变宿主细胞的胞内环境,逃脱宿主的免疫防御。许多胞内病原体利用细胞生理性的内吞囊泡途径侵染细胞,并适应了细胞内吞囊泡的酸化环境以达到其感染的目的。外源性的化学物质如氯化铵和氯喹等可以通过改变细胞内吞囊泡的酸化环境而抑制某些病毒和胞内寄生虫的感染,但宿主细胞是否存在相应的防御策略,内源性效应分子机器的身份以及调控网络一直是人们努力探究的重要问题
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Dis#
56
学习一下觉得非常好
85
#新策略#
60
#病原体#
67