超声诊断胎儿心脏多发性肿物一例
2019-02-24 徐晓旭 ,胡颖 ,范梅贞 中国超声医学
就诊原因:孕中期胎儿系统性超声检查。孕妇无不适感;无畸形家族史;早孕期胎儿NT检查未见异常;唐氏筛查为低风险。
患者:孕妇,28岁,临床孕周24.4周。
就诊原因:孕中期胎儿系统性超声检查。孕妇无不适感;无畸形家族史;早孕期胎儿NT检查未见异常;唐氏筛查为低风险。
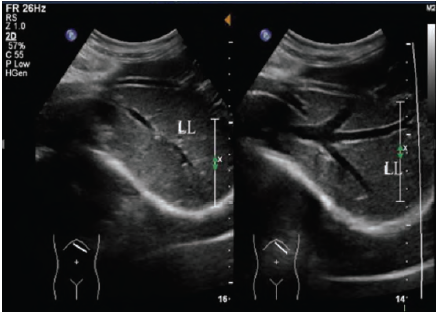
胎儿系统性超声检查:单活胎,超声孕周25.5周。
胎儿心脏超声表现如下:
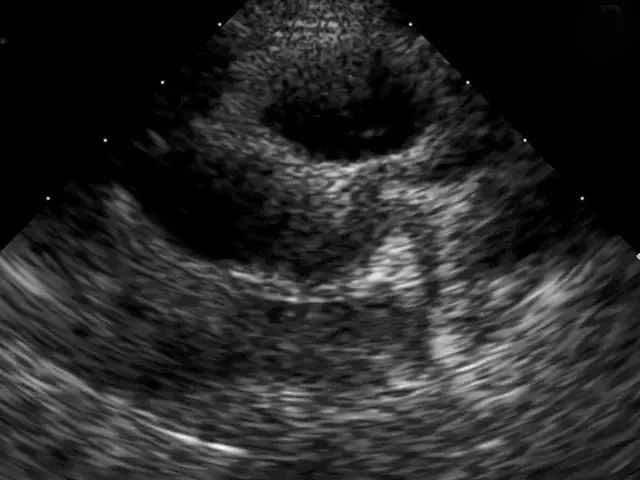
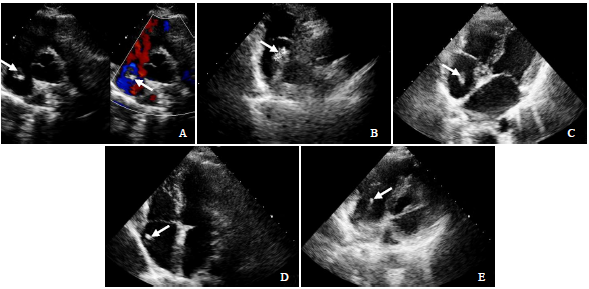
图1 胎儿左心室稍大,左心室腔内一均质强回声肿物,1.2x1.2cm,附着于左心室侧壁。
图2 左室流出道 可见部分肿物回声。
图3 左室流出道血流动力学改变不明显。
图4 右心房内均质强回声肿物,0.7x0.5cm。附着于右房顶部。
图5 右心房内肿物远离卵圆瓣。
图6心内两个强回声肿物。
胎儿超声诊断:胎儿多发心脏占位,心脏横纹肌瘤可能性大。
患者再次到上级医院行超声胎儿系统性筛查及胎儿心脏超声检查,诊断意见:胎儿多发心脏占位,心脏横纹肌瘤可能性大。由于肿瘤为多发,且左室内肿瘤瘤体较大,预后可能会很差。
讨论:
胎儿原发性心脏肿瘤罕见,活产婴儿心脏肿瘤的发生率约在0.0017%与0.028%之间。包括原发性良性心脏肿瘤和原发性恶性心脏肿瘤。其中绝大多数为良性疾病,最常见的是横纹肌瘤(cardiac rhabdomyoma ,CR),其他还包括畸胎瘤、纤维瘤、粘液瘤、血管瘤等。
心脏CR在原发性胎儿心脏肿瘤中最为常见,常为多发,是一种先天性多糖元肿瘤,典型的瘤细胞被称为“蜘蛛细胞”,多发心室内,90%呈多发性,形态稳定,通常深入心肌,也可附着室壁、瓣膜,或填塞心腔。肿瘤与周围心肌有明显的界限,但无真正的包膜,镜下横纹肌瘤由大的卵圆形细胞构成,胞质内具有丰富的糖元而构成空泡状,“蜘蛛细胞”是特征,而非真正的肿瘤,是由胎儿心脏的肌母细胞演化而来。
胎儿的CR与结节性硬化症(tuberous sclerosis,TSC)关系密切,60%~80%胎儿CR合并TSC,多发性CR患者几乎均合并TSC,单发性CR合并TSC几率尚不确定。TSC是一种常染色体显性遗传病,称为Bourneville病,可累及脑、皮肤、心脏、肾脏等多个器官,患儿预后差。
受母体激素水平变化的影响,约80%胎儿期发现的CR,在婴幼儿期可变小甚至完全消失。胎儿CR预后主要取决于胎儿心脏血流发动力学改变的程度及相关并发症。部分CR胎儿无特殊表现,肿瘤累及窦房结可引起心律失常,瘤体阻塞流出道或流入道,可引起胎儿水肿、心力衰竭等。
超声心动图检查是产前发现和随访胎儿CR的首选方法,横纹肌瘤的声像图的特点是结节状均匀强回声,多位于心室内,源于心室游离壁以及室间隔,多累及心脏左侧房室。
超声心动图较难鉴别CR是否合并TSC。出生后进行MRI检查TSC阴性的也不能予以排除。刘晓伟等研究结果显示,对于可疑TSC胎儿进行TSC基因检测可确诊。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#多发性#
56
#肿物#
72
#超声诊断#
47
#超声诊断#
47
学习了长知识
95
学习了新知识
108
学习了长知识
93
学习了新知识
100
学习了长知识
89
学习了新知识
55