CAR-T疗法明年有望进入临床应用
2016-12-24 佚名 腾讯科学
如果存在一种类似于灭癌银弹一样的东西,它将以你体内的那些癌细胞为唯一目标,而不会伤害你体内的其它细胞。这种展望来源于一种全新的免疫疗法,它被科学家们称为CAR-T细胞疗法。这种实验性癌症免疫疗法借助生物工程改造的细胞对癌细胞进行杀灭,而且以癌细胞为唯一目标。目前在全世界范围内有超多100多个CAR-T细胞疗法临床试验正在进行当中,美国食品和药品监督管理局有希望同意进行CAR-T细胞疗法。研究人员目
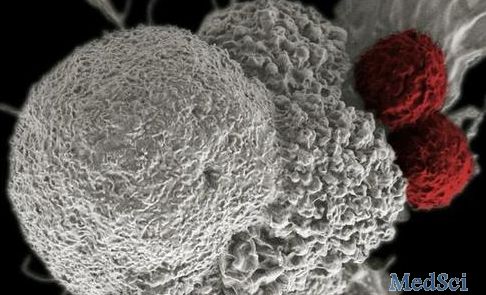
如果存在一种类似于灭癌银弹一样的东西,它将以你体内的那些癌细胞为唯一目标,而不会伤害你体内的其它细胞。这种展望来源于一种全新的免疫疗法,它被科学家们称为CAR-T细胞疗法。这种实验性癌症免疫疗法借助生物工程改造的细胞对癌细胞进行杀灭,而且以癌细胞为唯一目标。
目前在全世界范围内有超多100多个CAR-T细胞疗法临床试验正在进行当中,美国食品和药品监督管理局有希望同意进行CAR-T细胞疗法。研究人员目前已经看到了满意的效果,但是也出现了一些令人悲痛的结局,在这一年当中有5位秉着在进行治疗期间去世。
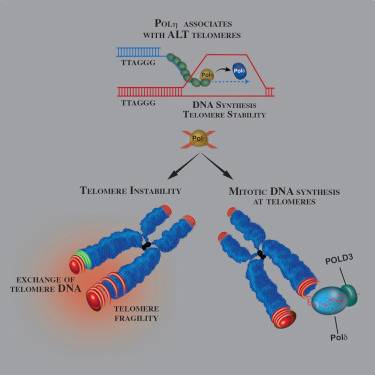
据加州大学圣迭戈分校摩斯癌症研究中心的Ezra Cohen教授称,当CAR-T疗法奏效时,它会通过引进一种定制的“生物学刺客”让身体的免疫系统对抗癌症。Cohen教授解释称:“这种疗法本质上是采用了一种正则细胞并且通过工程编辑使其对特定的目标进行攻击。”
西北纪念医院的一位肿瘤学家Jeffrey Sosman称:“目前来说,CAR-T细胞疗法并非癌症治疗的初步治疗,而是在患者初步治疗失败时进行的第二步治疗。但是随着技术的不断完善也可能会发生变化,但是这只是目前的治疗方式。”
病人需要身体足够健康才能承受CAR-T细胞疗法带来的一些潜在的健康影响。这种疗法带来的副作用在最糟糕的情况下会使患者的身体逐渐衰弱到死亡,还可能发生高烧、低血压、肿胀、肺水肿和心力衰竭等症状。这些症状都属于细胞激素释放症候群,这是一些免疫疗法中常见的有可能威胁生命的症状。
Cohen教授称:“充分发挥你的想象力,你可以开始想象免疫疗法未来将如何在许多领域取代外科手术,而且我认为对于许多病人来说,它将取代放射治疗和化学疗法。但是与此同时,我们将看到这种疗法将在许多方面与这些疗法相结合。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CAR-#
56
#临床应用#
52
期待有后续进展
84
还没完全搞懂原理
91
继续学习
102