JACC:生物降解药物洗脱支架植入后双重抗血小板治疗6个月与18个月比较
2017-06-20 xiangting MedSci原创
植入生物降解外用涂层的DES后,6个月DAPT的结果不劣于18个月DAPT。
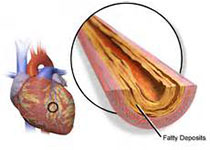
NIPPON研究(Nobori双重抗血小板治疗适当持续时间)是针对植入Nobori药物洗脱支架(DES)患者的短期与长期双重抗血小板治疗(DAPT)的非劣效性的多中心随机研究,这种支架具有生物降解的外用涂层。
对于生物降解聚合物涂层DES术后的患者,DAPT的最佳持续时间尚不清楚。
受试者为3,773例稳定或急性冠状动脉综合征而接受Nobori支架植入的患者。他们被按1:1随机分配接受6或18个月的DAPT治疗。主要终点是支架术后6-18个月的临床不良事件和脑血管事件(NACCE)(全因死亡率、心肌梗死、中风和大出血)。对3,307例随访了至少6个月的患者进行意向治疗分析。
34例(2.1%)接受短期DAPT和24例(1.5%)接受长期DAPT的患者发生NACCE(差异为0.6%,95%置信区间[CI]:1.5-0.3)。由于95%CI的下限在-2%的指定范围内,所以证实了短期DAPT的非劣效性。短期DAPT死亡率为1.0%,长期DAPT为0.4%,而心肌梗死分别为0.2%及0.1%,大出血为0.7%及0.7%。长期DAPT组NACCE的估计概率较低(风险比:1.44,95%CI:0.86-2.43)。
植入生物降解外用涂层的DES后,6个月DAPT的结果不劣于18个月DAPT。然而鉴于本研究的开放标签设计和非劣效性标准较宽,该结果仍需要谨慎解释。
原始出处:
Masato Nakamura,et al. Dual Antiplatelet Therapy for 6 Versus 18 Months After Biodegradable Polymer Drug-Eluting Stent Implantation.JACC. June 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
57
#支架植入#
86
#洗脱支架#
52
#药物洗脱支架#
72
#ACC#
70
#双重抗血小板治疗#
68
#植入#
53
学习了谢谢分享。
79