JCO:吸烟让结直肠癌幸存患者更接近死神
2015-02-05 佚名 生物谷
近日,刊登在国际杂志Journal of Clinical Oncology上的一篇研究论文中,来自国外的研究人员通过研究表明,相比不吸烟的结直肠癌幸存者而言,吸烟的患者死亡的风险是前者的2倍,这就揭示了吸烟和结直肠癌患者死亡直接相关,该研究为后期开发有效的干预措施来预防结直肠癌患者的死亡风险提供了一定的帮助。 文章中研究者对美国癌症协会癌症预防研究II期阶段中从18.4万成年人中诊断出
近日,刊登在国际杂志Journal of Clinical Oncology上的一篇研究论文中,来自国外的研究人员通过研究表明,相比不吸烟的结直肠癌幸存者而言,吸烟的患者死亡的风险是前者的2倍,这就揭示了吸烟和结直肠癌患者死亡直接相关,该研究为后期开发有效的干预措施来预防结直肠癌患者的死亡风险提供了一定的帮助。
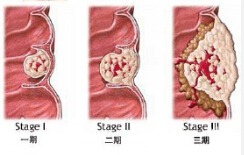
文章中研究者对美国癌症协会癌症预防研究II期阶段中从18.4万成年人中诊断出的2548名新发侵入性非转移性的结直肠癌患者进行调查分析,这些患者均为癌症幸存者,在随后的跟踪调查过程中有1074名个体存活平均7.5年,其中有453名患者因结直肠癌死亡。
研究者Peter Campbell博士表示,我们研究发现,诊断前吸烟者因各种原因而死亡的风险同患结直肠癌死亡的风险一样,都超过2倍,诊断前吸烟往往和较高的全因死亡率相关,但和结直肠癌相关的死亡率并无关系。诊断后吸烟往往会增加癌症患者至少2倍的死亡风险,而且和两倍的结直肠癌特异性死亡率直接相关。
对于吸烟者而言其机体往往更易出现恶性肿瘤,而吸烟同时也会降低结直肠患者疗法的效果,研究者最后说道,未来研究我们还将继续深入理解为何吸烟会增加结直肠癌特异性的死亡率,并且确定是否确诊癌症后戒烟可以有效降低结直肠癌患者的死亡率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCO#
65
学习了,学习了!
56
不错的文章,学习了
101
赞
200
已阅
149
已阅
100
还是不吸烟好
124
#结直肠#
58
吸烟对会儿街采等都有关注你一下但是需要区分一下到底是早期中期和晚期以及它的影响程度
113