DDS:经口内镜下肌切开术治疗失弛缓症患者的长期疗效分析
2019-04-21 不详 MedSci原创
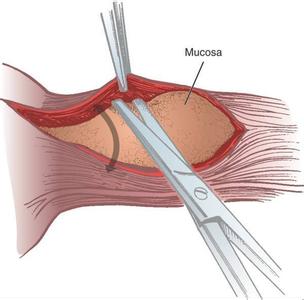
经口腔内镜下肌切开术在治疗贲门失弛缓症中有很大的作用,因此,本研究旨在评估经口腔内镜下肌切开术(POEM)对贲门失弛缓症患者的远期疗效。
背景及目的
经口腔内镜下肌切开术在治疗贲门失弛缓症中有很大的作用,因此,本研究旨在评估经口腔内镜下肌切开术(POEM)对贲门失弛缓症患者的远期疗效。
方法
研究人员回顾性分析了在浙江中医药大学第一附属医院接受POEM治疗的115例患者(中位年龄45岁)和中位随访36个月的前瞻性资料。主要观察结果为Eckardt评分和食道下端括约肌压力变化,并观察胃食管反流情况。
结果
研究结果显示所有患者的平均Eckardt评分从术前的7.5±1.9降至术后1个月的2.3±1.4(P<0.001)。治疗成功率为91.3%[95%CI:86.2-96.4]。所有患者中共发生16起(13.9%)手术失败,4例无反应者,8例早期复发(3个月至3年),4例晚期复发(3年后)。此外,21名(20.6%)患者在两年的随访期间出现反流症状。在随后的三年随访期间,仅新增了一名有症状反流的患者。此外,71例(61.7%)患者在POEM后接受胃镜检查,13例(18.3%)患者被诊断为反流性食管炎。
结论
POEM治疗贲门失弛缓症安全有效,具有良好的远期疗效。
原始出处:
Chenghai He. Et al. Long-Term Efficacy of Peroral Endoscopic Myotomy for Patients with Achalasia: Outcomes with a Median Follow-Up of 36 Months. Digestive Diseases and Sciences.2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#疗效分析#
58
#经口内镜下肌切开术#
59
#内镜#
56
#长期疗效#
52
谢谢梅斯提供这么好的信息,学到很多
66